Combining beta-blockers and calcium channel blockers sounds like a smart move-two drugs, one goal: lower blood pressure and protect the heart. But this combo isn’t as simple as adding two pills together. It’s like mixing two powerful engines. If tuned right, they work in harmony. Get it wrong, and you risk serious heart problems-slowed rhythms, fainting, even heart failure.
How These Drugs Work-And Why They’re Often Used Together
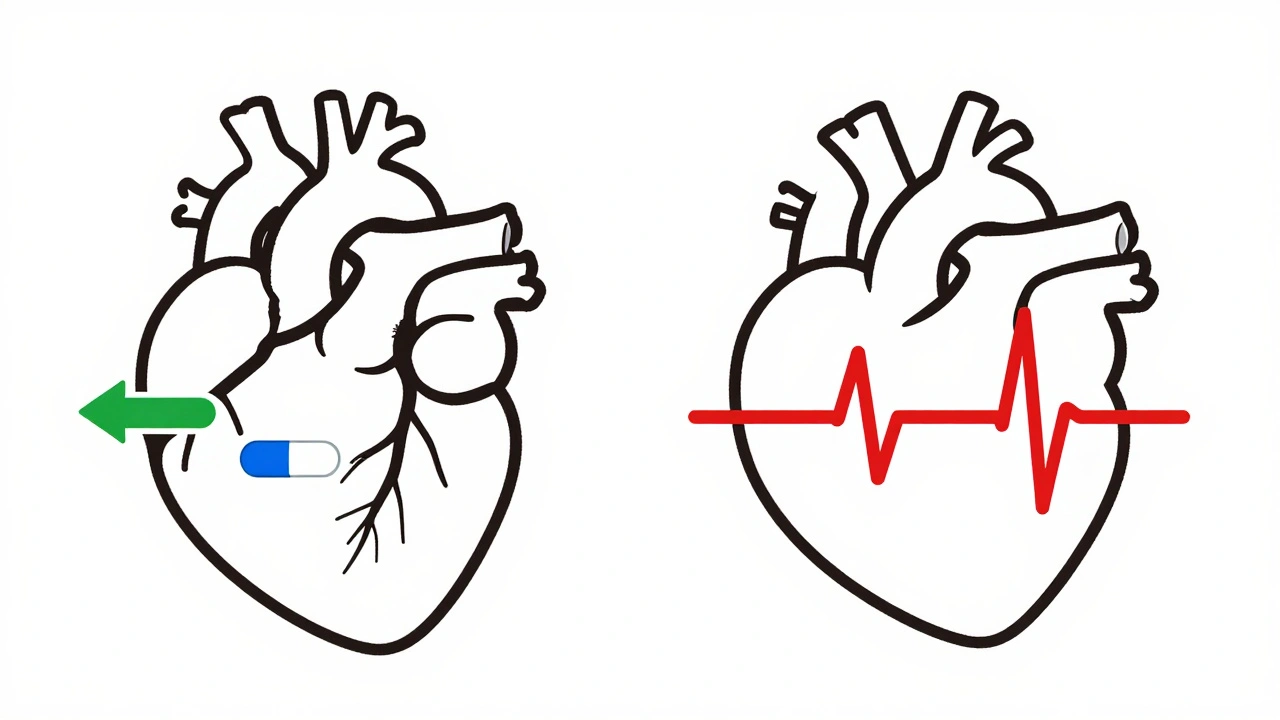
Beta-blockers, like metoprolol and carvedilol, slow the heart by blocking adrenaline. They reduce heart rate, lower blood pressure, and decrease how hard the heart pumps. Calcium channel blockers, such as amlodipine and diltiazem, relax blood vessels by stopping calcium from entering heart and artery cells. This also lowers blood pressure and can ease chest pain.
When used alone, both are effective. But when a patient’s blood pressure won’t budge with one drug, or they have both high blood pressure and angina, doctors sometimes add the second. The idea? Beta-blockers handle the heart’s workload, while calcium channel blockers open up the arteries. Together, they can do more than either alone.
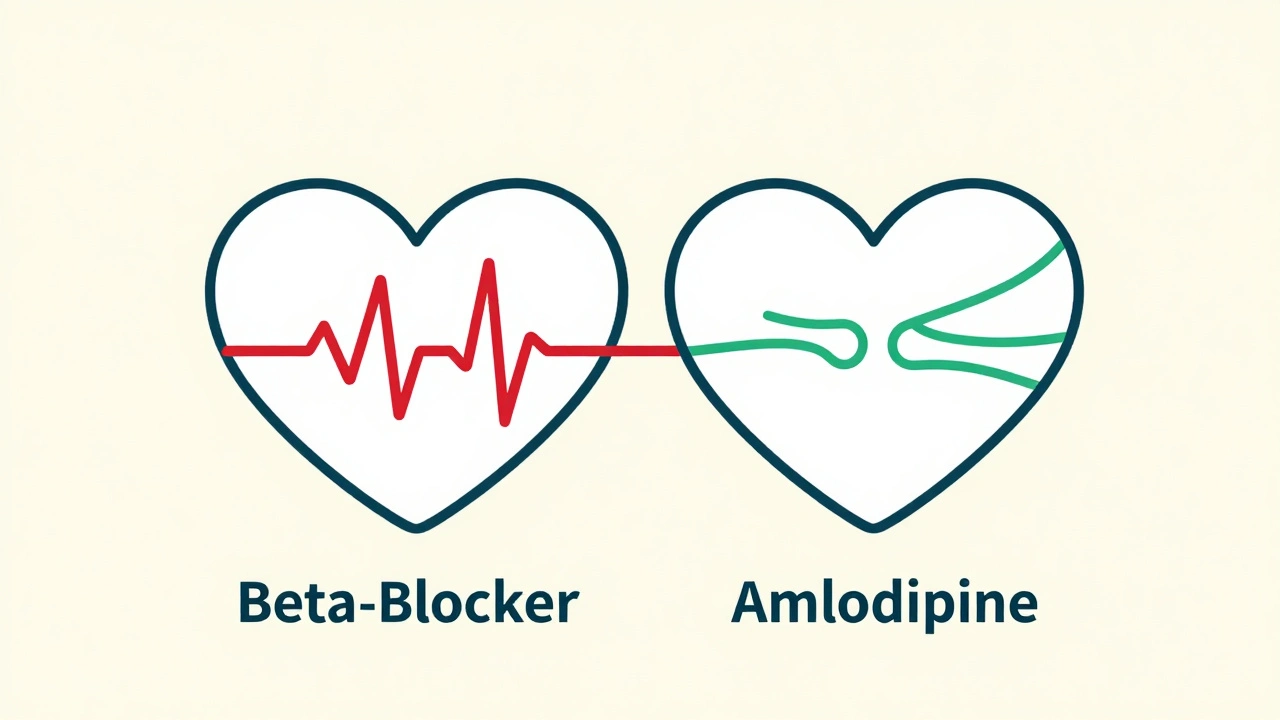
But here’s the catch: not all calcium channel blockers are the same. There are two main types, and they behave very differently when paired with beta-blockers.
The Big Divide: Dihydropyridines vs. Non-Dihydropyridines
Think of calcium channel blockers as two different tools. Dihydropyridines-like amlodipine and nifedipine-mostly affect blood vessels. They cause less direct impact on the heart’s rhythm or pumping ability. That makes them safer to pair with beta-blockers.
Non-dihydropyridines-verapamil and diltiazem-hit the heart harder. They slow the electrical signals that control heartbeat and reduce how strongly the heart contracts. When combined with beta-blockers, this effect multiplies. The result? A dangerous drop in heart rate, prolonged PR intervals on an ECG, and in severe cases, complete heart block.
Studies show that verapamil plus a beta-blocker causes significant bradycardia or heart block in 10-15% of patients. In older adults or those with existing conduction issues, the risk jumps even higher. One 2023 study found that patients on this combo had a 3.2-fold higher chance of needing a pacemaker than those on beta-blockers with amlodipine.
When the Combo Works-And Who Should Avoid It
This combination isn’t off-limits. In fact, the 2018 European Society of Cardiology guidelines still list it as a valid option-for the right patients.
It’s most commonly used in people with:
- Hypertension plus stable angina
- High resting heart rate (above 80 bpm)
- Chronic stable heart failure (only with specific beta-blockers like carvedilol or bisoprolol)
But it’s strictly avoided in patients with:
- Sinus node dysfunction
- Second- or third-degree heart block
- PR interval longer than 200 milliseconds
- Heart failure with reduced ejection fraction (especially with verapamil or diltiazem)
A 2022 analysis in the AHA Hypertension journal found that BB+verapamil increased the risk of heart failure hospitalization by nearly three times compared to BB+amlodipine. That’s not a small risk-it’s a red flag.
Real-World Outcomes: Benefits vs. Risks
It’s not all bad news. A large 2023 study of nearly 19,000 Chinese patients found that those on beta-blocker + dihydropyridine CCB combinations had:
- 17% lower risk of major heart events
- 22% lower stroke risk
- 28% lower chance of developing chronic heart failure
But here’s the key: these benefits were only seen with amlodipine, not verapamil. The same study showed verapamil combinations offered no advantage-and significantly higher risk.
Doctors report better outcomes with BB+amlodipine. One cardiologist from Massachusetts General Hospital noted that in over 200 patients, only 3% developed ankle swelling-a manageable side effect. Meanwhile, online forums are filled with warnings from physicians who’ve seen patients suffer complete heart block after adding verapamil to metoprolol.
Side Effects You Can’t Ignore
Even the safer combos come with trade-offs.
Peripheral edema (swelling in ankles or legs) is common with dihydropyridines like amlodipine. About 22% of patients on BB+amlodipine experience it, compared to 16% on other dual therapies. It’s usually mild and can be fixed by lowering the dose.
Bradycardia is the silent danger. A heart rate below 50 bpm might not feel like a problem-until it drops to 40, then 30. Patients may feel dizzy, fatigued, or pass out. In older adults, this can lead to falls or cardiac arrest.
Drug interactions are rare but possible. Verapamil can slow the metabolism of some beta-blockers, especially in people with a genetic variation (CYP2D6 poor metabolizers). This can raise beta-blocker levels by 20-30%, increasing side effects without any dose change.

How Doctors Decide-And What You Should Ask
Before starting this combo, a doctor should check:
- An ECG to measure PR interval and check for conduction delays
- An echocardiogram to assess heart pumping function (ejection fraction)
- Current medications to avoid hidden interactions
- Age, kidney function, and history of fainting or slow heart rhythms
After starting, patients need close follow-up: weekly heart rate and blood pressure checks for the first month. If the heart rate drops below 50 bpm or you feel lightheaded, call your doctor immediately.
Patients should ask:
- “Is this combination necessary, or is there a safer option?”
- “Am I on a dihydropyridine like amlodipine-or a non-dihydropyridine like verapamil?”
- “What signs should I watch for that mean I need to stop this?”
The Future of This Combo
Prescriptions for BB+CCB combinations make up about 12% of dual therapy use in the U.S., far behind ACE inhibitor + CCB or ACE inhibitor + diuretic. But adoption varies: in China, it’s used in 22% of cases.
Guidelines are shifting. The FDA added a boxed warning in 2021 for verapamil + beta-blocker combinations in patients with conduction problems. The European Medicines Agency now requires an echocardiogram before starting. Integrated health systems like Kaiser Permanente cut adverse events by 44% after implementing strict protocols.
Industry data predicts that BB+amlodipine prescriptions will grow 5.7% per year through 2028, driven by aging populations and better safety data. Verapamil combinations? They’re fading out.
This combo isn’t disappearing-it’s becoming more selective. The days of using it casually are over. Today, it’s reserved for specific cases, with strict monitoring and clear boundaries.
Can beta-blockers and calcium channel blockers be taken together safely?
Yes-but only under strict conditions. The combination is safe when using a dihydropyridine calcium channel blocker like amlodipine, especially in patients with high blood pressure and angina. It’s dangerous with non-dihydropyridines like verapamil or diltiazem, particularly in older adults or those with heart rhythm issues. Always get an ECG and echocardiogram before starting.
What’s the biggest risk of combining beta-blockers and calcium channel blockers?
The biggest risk is excessive slowing of the heart (bradycardia) or heart block, especially with verapamil or diltiazem. This can lead to dizziness, fainting, or even cardiac arrest. Studies show up to 15% of patients on this combo develop serious conduction problems, and the risk jumps in people over 65 or those with pre-existing heart rhythm issues.
Is amlodipine safer than verapamil when combined with a beta-blocker?
Yes, significantly. Amlodipine affects blood vessels more than the heart’s electrical system, so it’s much less likely to cause dangerous slowing of the heartbeat. Multiple studies show BB+amlodipine has better safety and similar or better outcomes than BB+verapamil. Verapamil combinations are now discouraged in most guidelines unless no other option exists.
What should I do if I start feeling dizzy or fatigued on this combo?
Stop taking the medication and contact your doctor immediately. Dizziness, extreme fatigue, or fainting can signal dangerously low heart rate or heart block. Don’t wait to see if it gets better. Your doctor will likely check your heart rhythm with an ECG and may adjust or stop one of the drugs.
Are there any tests I should ask for before starting this combination?
Yes. Ask for an electrocardiogram (ECG) to check your PR interval and heart rhythm, and an echocardiogram to measure your heart’s pumping ability (ejection fraction). These tests help identify hidden risks like conduction delays or weakened heart muscle. If you’re over 65 or have a history of fainting, these are non-negotiable.
Why do some doctors still prescribe verapamil with beta-blockers?
Some doctors may prescribe it out of habit, lack of awareness of newer data, or because they’re treating a patient with severe angina who hasn’t responded to other options. But current guidelines and clinical evidence strongly favor amlodipine instead. Most cardiologists now avoid verapamil + beta-blocker combos unless there’s no alternative-and even then, they monitor closely.
Final Thoughts: Less Is More
This combination isn’t a first-line fix. It’s a targeted tool for specific cases. The trend is clear: doctors are moving away from verapamil and diltiazem with beta-blockers. Amlodipine is becoming the preferred partner. The key isn’t adding more drugs-it’s choosing the right ones.
If you’re on this combo, know which type of calcium channel blocker you’re taking. Ask questions. Track your pulse. Don’t ignore symptoms. The goal isn’t just to lower blood pressure-it’s to keep your heart healthy, not just quieted.

Written by Felix Greendale
View all posts by: Felix Greendale