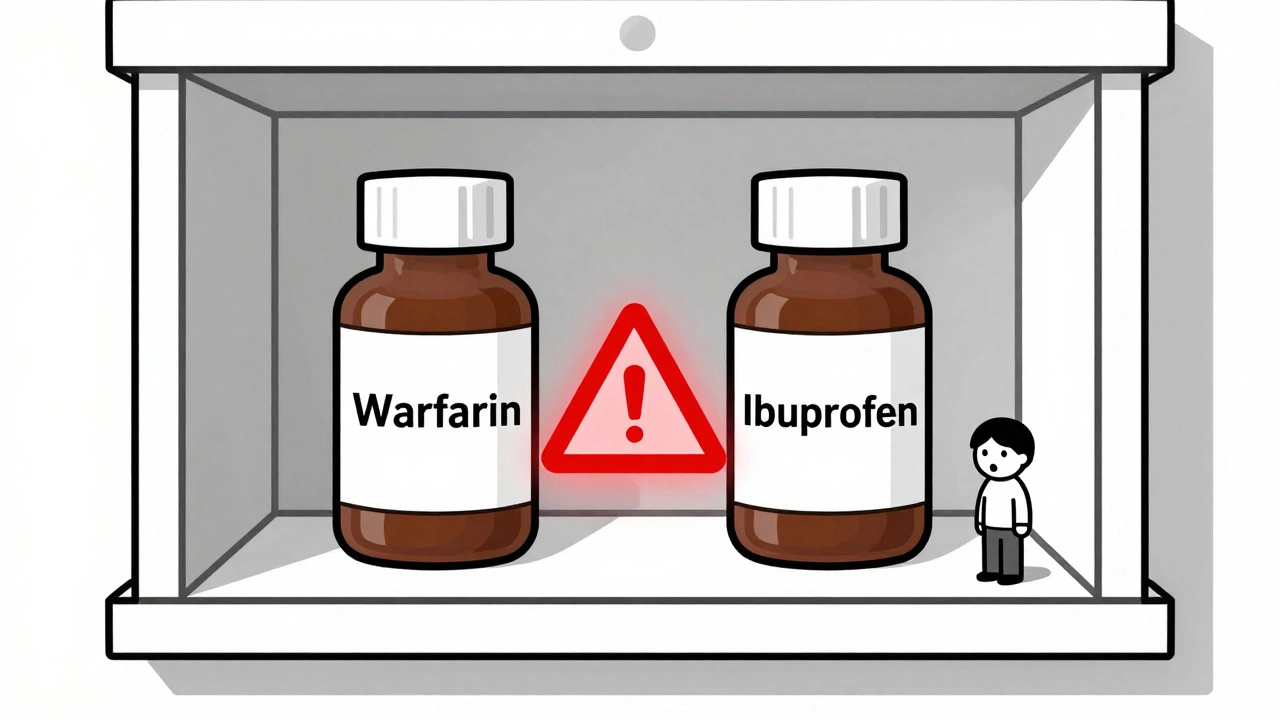
Combining blood thinners with common painkillers like ibuprofen or naproxen isn’t just a bad idea-it’s dangerous. Every year, thousands of people end up in the hospital because of this exact mix. And most of them had no idea it was risky. If you’re on a blood thinner-whether it’s warfarin, apixaban, rivaroxaban, or another-taking an NSAID for a headache, back pain, or arthritis could be putting your life at risk.
What Happens When Blood Thinners Meet NSAIDs?
Blood thinners don’t actually make your blood thinner. They stop it from clotting too easily. That’s crucial if you have atrial fibrillation, a history of blood clots, or a mechanical heart valve. But NSAIDs-like ibuprofen, naproxen, and diclofenac-do something else entirely. They block enzymes in your body called COX-1 and COX-2. That reduces pain and swelling, but it also messes with your platelets, the tiny cells that help blood clot. When you take both together, your body loses two layers of protection against bleeding. The blood thinner slows down clotting factors. The NSAID stops platelets from sticking together. The result? A perfect storm for uncontrolled bleeding. A massive 2024 study from Denmark tracked over 51,000 people on blood thinners. Those who also took NSAIDs were more than twice as likely to be hospitalized for bleeding. And it wasn’t just stomach bleeds. The risk jumped for bleeding in the brain (over three times higher), lungs, urinary tract, and even internal organs. One in three of these patients developed severe anemia from hidden blood loss.Not All NSAIDs Are Equal
If you think all over-the-counter painkillers are the same, you’re wrong. The risk varies widely:- Naproxen: 4.1 times higher risk of bleeding
- Diclofenac: 3.3 times higher risk
- Ibuprofen: 1.79 times higher risk
It Doesn’t Matter What Blood Thinner You’re On
Many people assume newer blood thinners like apixaban or rivaroxaban are safer than warfarin. That’s true in some ways-they don’t need constant blood tests. But when it comes to mixing with NSAIDs? No difference. The Danish study found the same spike in bleeding risk whether patients were on warfarin or one of the DOACs. That means if you’re on Eliquis, Xarelto, Pradaxa, or Savaysa, you’re just as vulnerable. There’s no "newer = safer" loophole here. The interaction is class-wide.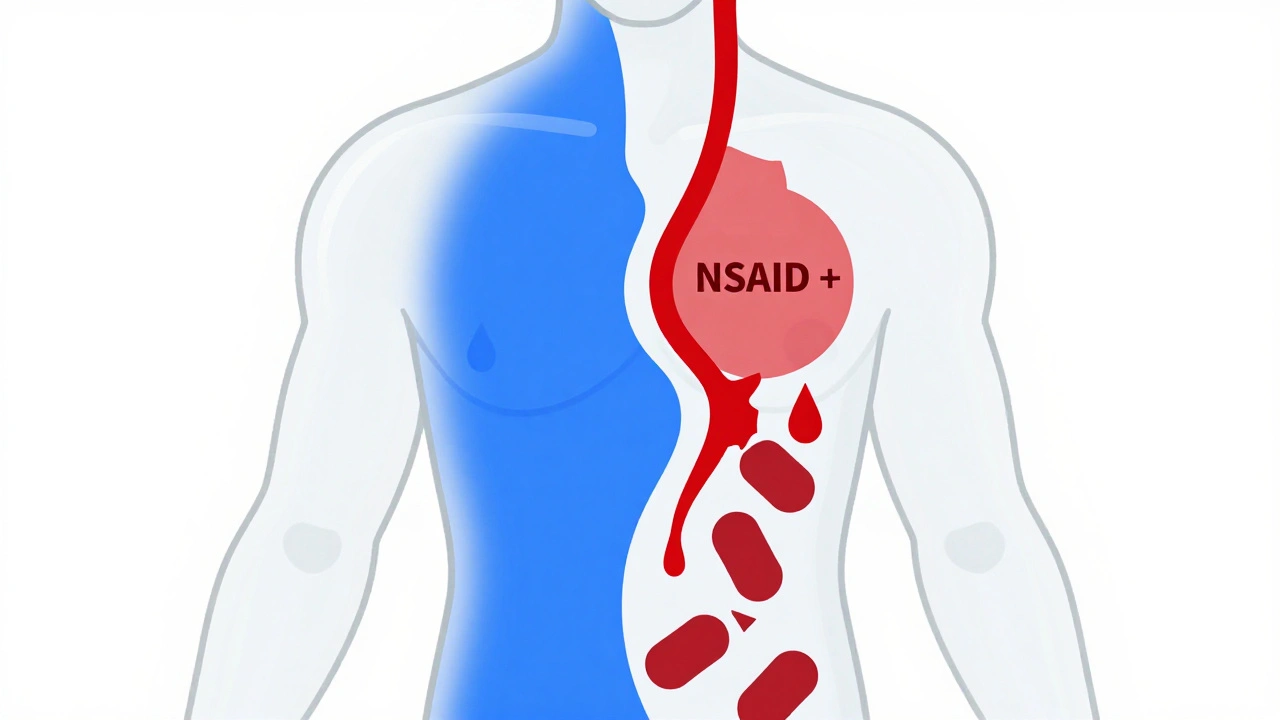
Why People Don’t Realize the Danger
Most patients don’t think of ibuprofen as a "drug"-they see it as a pain reliever, like aspirin. But aspirin is also an NSAID. And if you’re on a blood thinner, you’ve probably been told to avoid it. So why do people still take ibuprofen? It’s because the warnings aren’t clear enough. Pharmacies don’t always flag it. Doctors don’t always ask. Patients don’t always remember to mention they took a Tylenol for a headache-or a naproxen tablet for a sore knee. And many assume if it’s sold over the counter, it’s harmless. But here’s the truth: NSAIDs are one of the top causes of drug-related hospitalizations in older adults. And when combined with anticoagulants, the risk skyrockets.What You Should Take Instead
If you need pain relief while on a blood thinner, there’s one clear winner: acetaminophen (Tylenol). Unlike NSAIDs, acetaminophen doesn’t affect platelets or the stomach lining. It doesn’t interfere with clotting. It’s not perfect-it can harm your liver if you take too much-but at recommended doses, it’s the safest choice for people on blood thinners. For chronic pain-like arthritis or back pain-consider non-drug options:- Heat packs or ice therapy
- Physical therapy
- Low-impact exercise like swimming or walking
- Topical creams with menthol or capsaicin
What If You Absolutely Need an NSAID?
Sometimes, there’s no alternative. Maybe you’re having a flare-up of gout or severe inflammation that acetaminophen can’t touch. In those rare cases, your doctor might approve a short-term, low-dose NSAID. But even then:- Use the lowest dose possible
- Take it for the shortest time possible-no more than a few days
- Avoid daily use at all costs
- Don’t combine with alcohol
- Ask about a proton pump inhibitor (like omeprazole) to protect your stomach-but know this doesn’t stop bleeding elsewhere
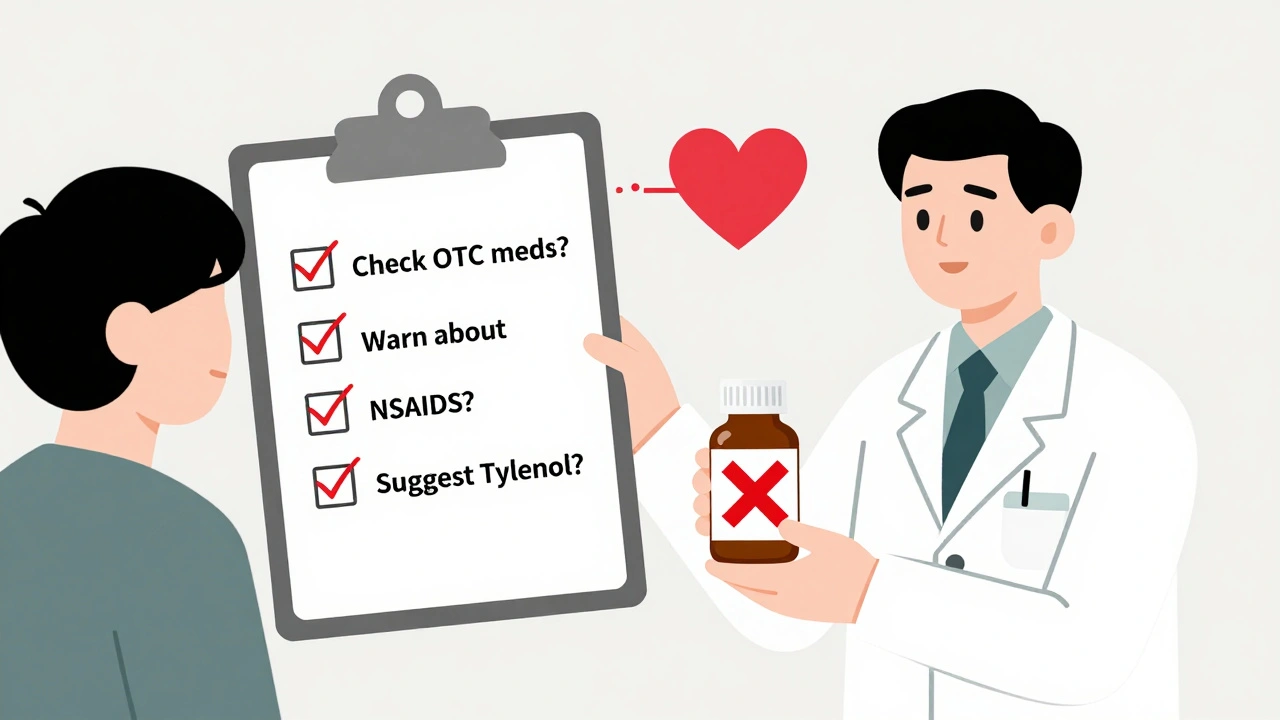
What Your Doctor Should Be Doing
This isn’t just your problem to manage alone. Doctors need to be proactive. At every visit, they should ask: "Are you taking any painkillers, even over-the-counter ones?" Not just "Do you take ibuprofen?"-because people forget to mention it. They need to check your medication list every time, including supplements and herbal products. Health systems should be building alerts into electronic records. If a patient is prescribed warfarin or apixaban, the system should flag any NSAID order-and remind the prescriber to consider alternatives. And if you’re on a blood thinner, you have the right to ask: "Is this painkiller safe with my medication?" Don’t assume the answer is yes.The Bigger Picture
This isn’t a rare edge case. In the U.S. alone, over 30 million prescriptions for ibuprofen are written every year. Add in the billions of OTC tablets, and you’re looking at tens of millions of people who might be mixing it with blood thinners. Meanwhile, about 3 to 6 million Americans are on anticoagulants. The combination is common. And the consequences are severe. That’s why the American College of Cardiology called this a "public health challenge"-and why experts are pushing for better education, clearer labels, and smarter prescribing. You don’t need to live in fear. But you do need to be informed. If you’re on a blood thinner, treat every NSAID like a loaded gun. Even one pill can tip the scales.What to Do Right Now
- Check your medicine cabinet. Do you have ibuprofen, naproxen, or diclofenac? If so, and you’re on a blood thinner, don’t use them.
- Call your pharmacist. Ask them to review all your medications-including supplements and OTC drugs.
- Bring a list of everything you take to your next doctor visit. Include herbal teas, CBD oil, and pain patches.
- Switch to acetaminophen for pain relief. Stick to 3,000 mg or less per day unless your doctor says otherwise.
- If you’ve taken an NSAID in the last week and notice unusual bruising, dark stools, dizziness, or shortness of breath, get checked immediately.
Can I take ibuprofen with warfarin?
No. Taking ibuprofen with warfarin increases your risk of serious bleeding by nearly 80%. Even occasional use can trigger internal bleeding in the stomach, brain, or elsewhere. Acetaminophen is the safer pain relief option. If you must use ibuprofen, only do so under direct medical supervision and for no more than a few days.
Is naproxen worse than ibuprofen with blood thinners?
Yes. Naproxen increases bleeding risk by more than four times compared to blood thinners alone-nearly double the risk of ibuprofen. It’s longer-acting and more strongly inhibits platelet function. Avoid naproxen entirely if you’re on a blood thinner. Diclofenac is similarly dangerous.
Are newer blood thinners safer with NSAIDs?
No. Whether you’re on warfarin, apixaban, rivaroxaban, dabigatran, or edoxaban, combining any of them with NSAIDs raises your bleeding risk by the same amount. The type of blood thinner doesn’t matter-what matters is the NSAID. All anticoagulants interact dangerously with NSAIDs.
Can I take aspirin with blood thinners?
Aspirin is an NSAID and should not be taken with blood thinners unless specifically prescribed by your doctor for heart protection. Even low-dose aspirin (81 mg) increases bleeding risk. Never take aspirin for pain if you’re on a blood thinner without medical approval.
What should I do if I accidentally took an NSAID?
If you took one dose of an NSAID by accident, don’t panic-but monitor yourself closely. Watch for signs of bleeding: unusual bruising, black or tarry stools, blood in urine, dizziness, or shortness of breath. Contact your doctor or pharmacist immediately. Do not take another dose. In the future, keep a list of safe and unsafe medications next to your pill organizer.
Can I use topical NSAIDs like gels or creams?
Topical NSAIDs (like diclofenac gel) are absorbed through the skin and enter the bloodstream in smaller amounts. While they’re less risky than oral NSAIDs, they still carry some bleeding risk-especially if used on large areas, for long periods, or with other blood thinners. They’re not risk-free. Acetaminophen or non-drug therapies are still safer choices.
How do I tell my doctor I’ve been taking ibuprofen without sounding careless?
Say it plainly: "I’ve been taking ibuprofen for my knee pain because I didn’t realize it could be dangerous with my blood thinner. I want to stop safely-what should I use instead?" Most doctors appreciate honesty. They’ve seen this before. The goal is to fix the problem, not judge you.

Written by Felix Greendale
View all posts by: Felix Greendale