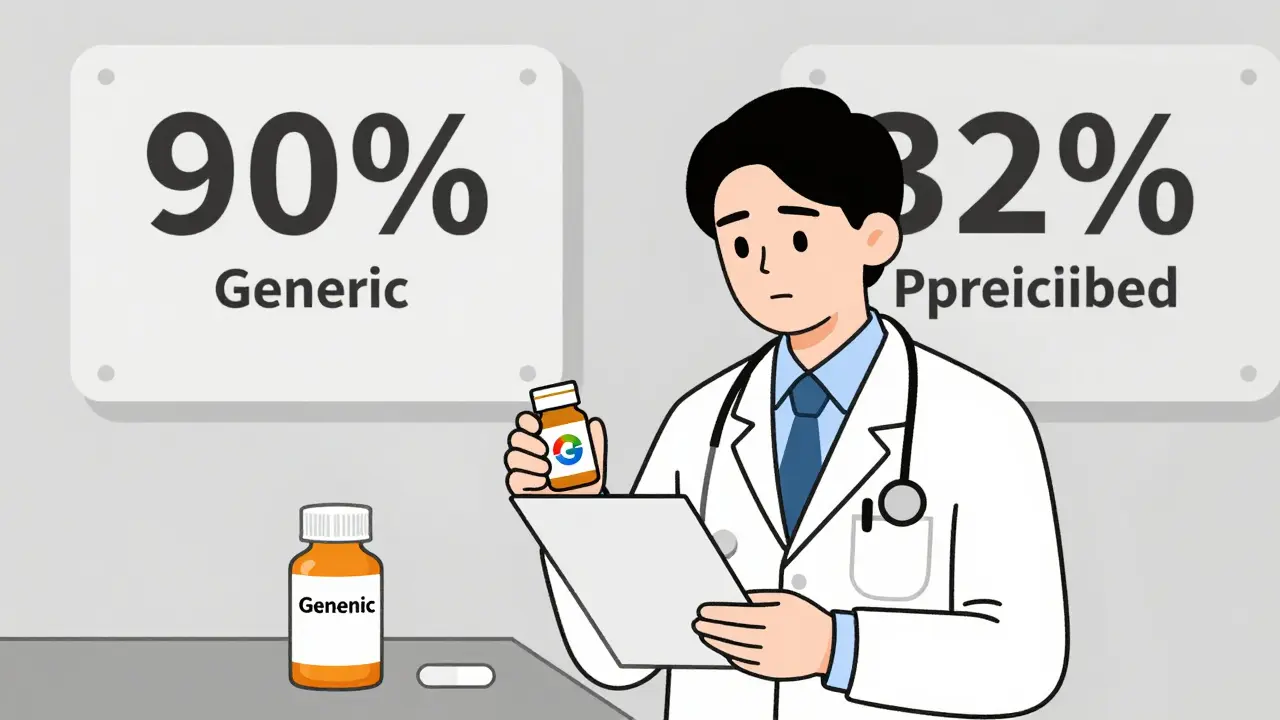
Doctors prescribe generic drugs every day-but do they truly believe they work as well as brand-name pills? The answer isn’t simple. Behind the statistics lies a quiet tension: generics make up 90.1% of all U.S. prescriptions, yet only 32.7% of physicians routinely prescribe them as first-line treatment. Why the gap?
Many Doctors Still Doubt Generic Effectiveness
Despite decades of regulatory approval and billions in cost savings, a significant number of physicians still question whether generic drugs are truly equivalent. A 2017 study of 134 Greek doctors found that more than 25% believed generics were less effective than brand-name versions. Even more troubling, 27.3% of physicians doubted therapeutic equivalence outright. These aren’t fringe opinions-they’re common enough to shape real-world prescribing habits. The belief that generics are inferior isn’t just about cost. Some doctors report seeing patients experience worse side effects after switching. One physician in a CDC rural study recalled a patient who stopped taking their generic thyroid medication because they felt "more jittery"-even though lab tests showed normal hormone levels. The patient didn’t trust the drug, and the doctor didn’t push back. That’s the problem: when providers hesitate, patients pick up on it.Age, Experience, and Specialization Matter
Not all doctors think the same way. Older physicians, those with over 10 years of experience, and specialists are far more skeptical than younger, general practitioners. In the same Greek study, male doctors were significantly more likely to reject generics than female colleagues. This isn’t about gender alone-it’s about training, exposure, and ingrained habits. Specialists, particularly in cardiology and neurology, are the most cautious. Drugs like warfarin and levothyroxine have narrow therapeutic windows. A small change in absorption can mean the difference between effective treatment and dangerous side effects. Reddit threads from practicing physicians show that 62.3% of respondents have seen at least one adverse event they believe was caused by switching generics for these drugs. That kind of experience sticks. Meanwhile, primary care doctors-who see the highest volume of patients-are often caught between policy pressure to cut costs and real-world uncertainty. One GP in Oxford’s 2023 study admitted: "I want to prescribe generics. But if a patient comes back with weird symptoms, I can’t tell if it’s the drug, the disease, or just bad timing. That uncertainty makes me stick with what I know."Knowledge Gaps Are Real-Even Among Experts
You’d think doctors who prescribe medications daily would know the science behind generics. But they don’t. Only 43.7% of primary care physicians correctly understood the FDA’s bioequivalence standards (80-125% absorption range). Yet 78.4% claimed they were "familiar" with regulatory requirements. That’s a dangerous mismatch. Many assume generics must be "stronger" to work, leading to fears of overdosing. Others think different manufacturers produce inconsistent batches. In reality, the FDA requires every generic to meet the same quality standards as brand-name drugs. But without clear, ongoing education, those facts get lost. The evidence is clear: when doctors understand how generics are tested, their confidence grows. A 90-minute educational workshop in Greece led to a 37.2% increase in positive attitudes toward generics-and a 22.5% jump in actual prescribing over six months. The biggest boost? Among doctors with 5-10 years of experience. Not the veterans. Not the rookies. The ones still forming their habits.
Pharmacists Know Better-And It Shows
Here’s a striking contrast: pharmacists are far more confident in generics than physicians. Studies show only 22.1% of pharmacists doubted therapeutic equivalence, compared to 28.7% of doctors. Why? Because pharmacists are trained to evaluate formulations, not just symptoms. They see the chemistry. They handle the batches. They know the manufacturing audits. Yet doctors rarely consult them. In most clinics, the pharmacist is an afterthought. If a doctor prescribes a brand-name drug because they "don’t trust the generic," the pharmacist often doesn’t get a chance to explain why that’s unnecessary. That’s a missed opportunity. In countries like Germany, where pharmacists have more authority in substitution, generic use is 18.4% higher than in the U.S.The Real Barrier Isn’t the Drug-It’s the Conversation
The biggest problem isn’t science. It’s communication. A staggering 68.4% of patients learn about generic drugs from their doctors. That means every time a physician says, "This is the same, just cheaper," without explaining why, they’re planting doubt. Patients hear "cheaper" and think "worse." They don’t know about bioequivalence testing. They don’t know that the same company often makes both the brand and generic versions. They don’t know that the FDA inspects generic factories as rigorously as brand-name ones. In rural clinics, this lack of trust spirals. 41.7% of patients who were switched to generics without clear explanation stopped taking their meds altogether. That’s not just a medication issue-it’s a trust issue. And once trust is broken, it’s harder to rebuild.

Written by Felix Greendale
View all posts by: Felix Greendale