Exemestane Long-Term Risk Calculator
Assess Your Risk Factors
This tool helps evaluate your personal risk for common long-term effects after Exemestane treatment. Based on your inputs, it will show your risk level for key side effects.
Finishing a course of Exemestane is a relief, but many patients wonder what comes next. The drug hangs around in your system for a while, and its impact on hormones can echo years after the last dose. This guide breaks down the most common long‑term effects, how to spot them, and practical steps to keep your health on track.
Key Takeaways
- Exemestane works by blocking the enzyme that makes estrogen, which can lead to bone loss and joint discomfort over time.
- Typical long‑term issues include osteoporosis, hot flashes, joint pain, and subtle changes in heart health.
- Regular screening-bone density tests, lipid panels, and cognitive checks-helps catch problems early.
- Lifestyle tweaks such as weight‑bearing exercise and calcium‑rich nutrition can blunt many side effects.
- Contact your oncologist promptly if you notice sudden memory lapses, severe joint swelling, or unusual heart rhythm.
What Is Exemestane?
Exemestane is a prescription medication classified as an Aromatase inhibitor. It is primarily used after surgery or radiation to treat hormone‑responsive Breast cancer in post‑menopausal women. By shutting down the aromatase enzyme, the drug dramatically lowers circulating Estrogen levels, starving cancer cells that rely on this hormone to grow.
How Does Exemestane Work?
The aromatase enzyme sits mostly in fat tissue and converts androgens into estrogen. Exemestane binds irreversibly to this enzyme, meaning the body has to produce new enzyme proteins before estrogen production can resume. The result is a rapid drop-often up to 90%-in estrogen, which is great for halting tumor growth but also sets the stage for several hormonal side effects that can linger.
Long‑Term Effects You Might Notice
Most research follows patients for up to five years after treatment, and a handful of effects can stretch beyond that window. Below is a rundown of the most frequently reported issues, paired with real‑world numbers when available.
Bone Health: Osteoporosis and Fracture Risk
Reduced estrogen weakens the bone‑remodeling cycle, leading to lower bone mineral density (BMD). Studies show a 2‑4% annual loss in BMD for women on aromatase inhibitors, translating to a 10‑15% higher fracture risk after five years.
Joint and Muscle Discomfort
About 30‑40% of users report arthralgia-persistent joint pain-often worst in the knees, hips, and wrists. The pain can be dull or sharp, sometimes mimicking arthritis.
Hot Flashes and Night Sweats
Even after stopping the drug, sudden vasomotor episodes linger for up to two years in roughly a quarter of patients.
Cardiovascular Changes
Long‑term Lipid profiles may shift, with a modest rise in LDL cholesterol observed in 12% of survivors. The clinical significance varies, but it’s a cue for regular heart‑health checks.
Cognitive Changes
Minor memory lapses or “brain fog” have been noted in 15% of women, usually improving within a year but sometimes persisting.
Skin and Hair Alterations
Dry skin, thinning hair, and occasional nail brittleness appear in small percentages (5‑10%). While not dangerous, they affect quality of life.
Emotional Well‑Being
Hormone shifts can amplify anxiety or depressive symptoms. Around 10% of patients seek counseling for mood changes after completing therapy.
Incidence Table of Common Long‑Term Effects
| Effect | Reported Incidence | Typical Onset (Months) | Duration (Months) |
|---|---|---|---|
| Osteoporosis / Low BMD | 12‑18% | 6‑12 | Variable, may be chronic |
| Joint Pain (Arthralgia) | 30‑40% | 3‑9 | 6‑24 |
| Hot Flashes | 22‑28% | 1‑6 | 12‑24 |
| Elevated LDL Cholesterol | 12% | 6‑12 | Variable |
| Cognitive Fog | 15% | 2‑8 | 12‑18 |
Monitoring and Managing After Treatment
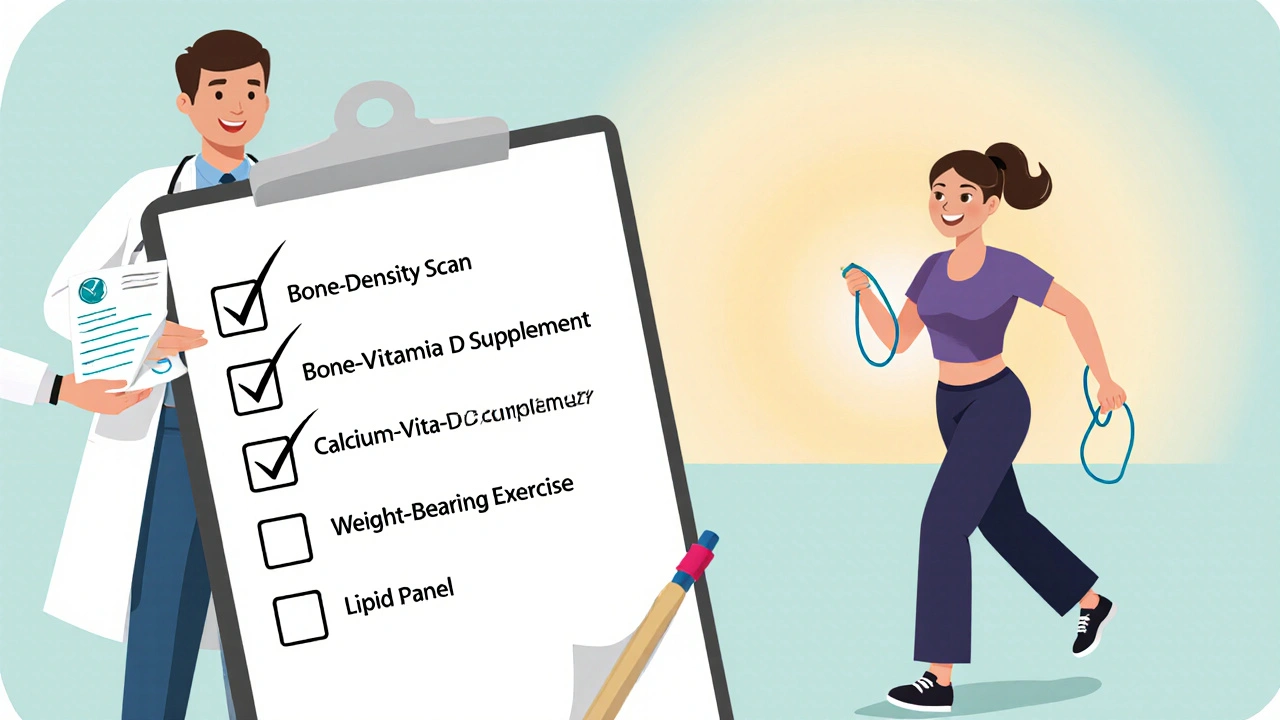
Staying ahead of these effects starts with a solid follow‑up plan. Here’s a practical checklist you can discuss with your oncologist or primary‑care doctor:
- Bone Health: Schedule a DEXA scan at the end of therapy, then every 1‑2 years. If BMD is low, consider calcium (1,200mg) and vitaminD (800‑1,000IU) supplements, plus weight‑bearing exercise like brisk walking or resistance bands.
- Joint Management: Over‑the‑counter NSAIDs (ibuprofen 400mg) can help, but talk to your doctor first. Physical therapy focusing on low‑impact stretching often reduces pain.
- Hot Flash Relief: Lifestyle tweaks-cool bedroom, layered clothing, avoiding caffeine and alcohol-make a difference. Some patients benefit from low‑dose antidepressants (e.g., venlafaxine 37.5mg) prescribed off‑label.
- Heart Checks: Get a lipid panel annually. If LDL climbs above 130mg/dL, a statin may be recommended.
- Cognitive Support: Simple brain‑training apps, regular aerobic activity, and adequate sleep (7‑8hours) aid recovery.
- Mental Health: If anxiety or low mood persists beyond three months, ask about counseling or a brief course of SSRIs.
Remember, exemestane side effects aren’t inevitable. Early detection and proactive care often keep them mild.
When to Call Your Doctor
- Sudden, severe joint swelling or inability to move a limb.
- Persistent hot flashes that disrupt sleep more than two nights a week.
- New‑onset chest pain, palpitations, or shortness of breath.
- Noticeable memory gaps that interfere with daily tasks.
- Signs of a fracture-sharp back pain after a minor fall or unexplained height loss.
Prompt medical attention can prevent complications and adjust your follow‑up plan accordingly.
Frequently Asked Questions
Will my cancer come back after stopping Exemestane?
The drug’s main job is to lower estrogen, which reduces the chance of recurrence. Most studies show a lower relapse rate for the first five years after therapy, but long‑term vigilance with regular scans remains essential.
Can I become pregnant after using Exemestane?
Exemestane is intended for post‑menopausal women, so pregnancy is unlikely. If you’re pre‑menopausal and taking the drug, discuss contraception with your doctor-its estrogen‑lowering effect can affect fertility.
How long does it take for bone density to improve after stopping the medication?
Bone rebuilding is slow. With calcium, vitaminD, and weight‑bearing exercise, many women see a 1‑2% BMD increase per year. Bisphosphonates can speed this up if a doctor prescribes them.
Are hot flashes permanent?
For most, they fade within 12‑24 months after stopping Exemestane. Lifestyle changes and, if needed, medication can shorten the duration.
Should I continue taking supplements after therapy ends?
Calcium (1,200mg) and vitaminD (800‑1,000IU) are generally recommended for life after aromatase inhibitor therapy, especially if bone density is low. Your doctor can tailor dosages.


Written by Felix Greendale
View all posts by: Felix Greendale