Every year, Americans fill over 3.9 billion prescriptions. Ninety percent of them are for generic drugs. And yet, those same generics cost just 12 percent of what brand-name drugs do. That’s not a typo. It’s the reality of how generics reshape the U.S. healthcare system - not with flashy marketing, but with hard numbers that save billions.
How Much Are You Really Saving?
In 2024, generic and biosimilar medicines saved the U.S. healthcare system $467 billion. That’s more than the entire annual budget of the Department of Education. For the average person, this isn’t abstract. If you take a monthly prescription, you’re likely paying $6.95 for a generic - compared to $28.69 for the brand-name version. That’s nearly five times cheaper. For someone on three prescriptions a month, that’s over $600 saved per year, just on out-of-pocket costs.
And it gets sharper for people without insurance. In 2019, a brand-name drug cost an uninsured patient an average of $87.20 per prescription. By 2024, that number had jumped to $130.18 - a 50 percent increase. Meanwhile, the cost of the generic version for the same drug dropped by $2.45. While brand-name companies raised prices, generics kept getting cheaper. That’s the opposite of what you’d expect in any other market.
Generics Aren’t Just Cheap - They’re Deflating the Market
Most industries see prices rise as demand grows. Generics do the opposite. Since 2019, the total amount spent on all generic drugs in the U.S. has gone down by $6.4 billion - even though more prescriptions are being filled. In 2015, Americans took about 167 billion generic pills. By 2024, that number climbed to 197 billion. More people using generics. Less money being spent. That’s deflation in action.
Take Vasostrict, a drug used for shock and low blood pressure. In just three months in 2025, its list price dropped by 76 percent. That’s not an anomaly. It’s a pattern. When a generic enters the market, competition drives prices down - often to pennies per pill. One study found that after a generic version of a drug became available, prices fell by an average of 80 percent within a year. That’s why generics make up only 12 percent of drug spending, even though they’re used in 9 out of 10 prescriptions.
Biosimilars Are the New Frontier
Biosimilars are the next wave. These aren’t copies of simple pills - they’re complex versions of biologic drugs used to treat cancer, arthritis, and autoimmune diseases. They cost less because they don’t need to repeat expensive clinical trials. In 2024, biosimilars saved $20.2 billion - nearly double the savings from the year before. Since their debut in 2015, they’ve saved the system $56.2 billion total. And over 3.3 billion days of patient therapy have passed with no unique safety issues reported.
Here’s the kicker: 60 percent of all biosimilar savings happened in just the last two years. Adoption is accelerating. More doctors are prescribing them. More insurers are covering them. And patients are getting the same effectiveness - at a fraction of the cost. A biosimilar for Humira, for example, can cost under $5,000 per year instead of $20,000. That’s not a small difference. It’s life-changing for people who need lifelong treatment.

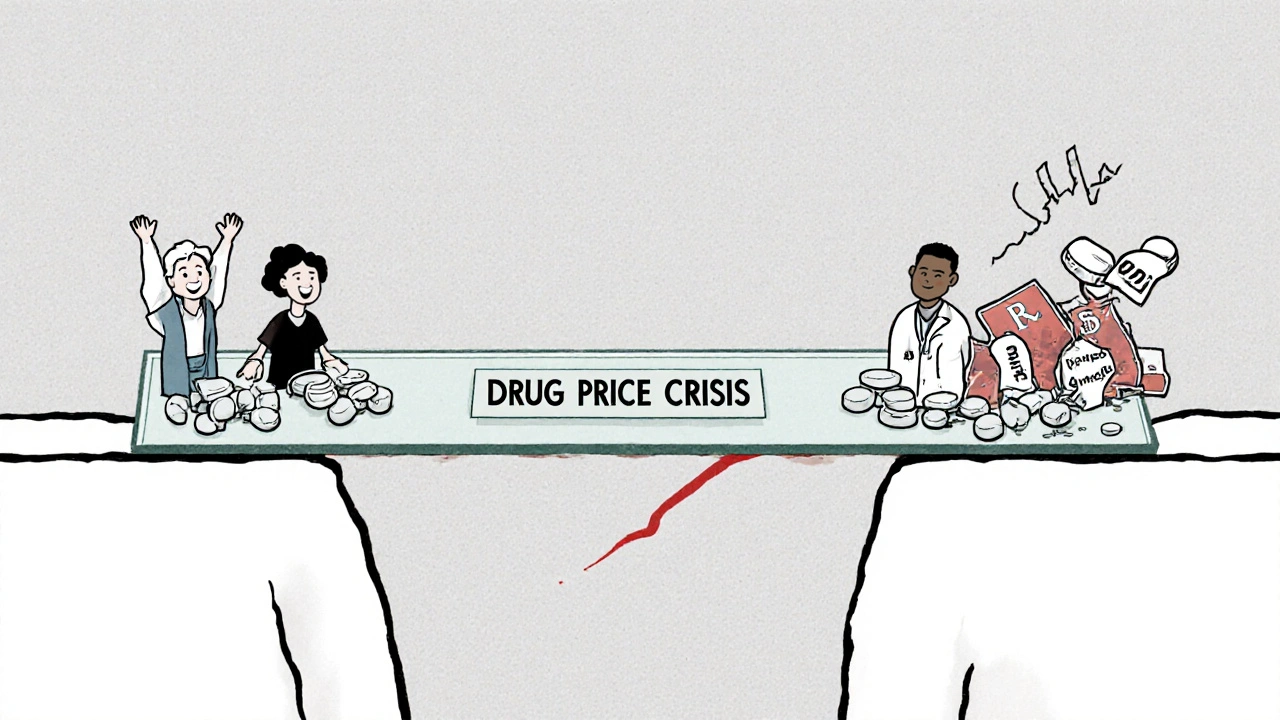
Why Are Brand-Name Drugs So Expensive?
Brand-name drugs make up only 10 percent of prescriptions but account for 88 percent of total drug spending. In January 2025, major pharmaceutical companies raised prices on 250 drugs by a median of 4.5 percent - more than double the overall inflation rate. Meanwhile, generic prices kept falling. Why the gap?
It’s not about R&D. Most brand-name drugs have long passed their patent expiration. The high prices are maintained through tactics like “product hopping” - where companies slightly tweak a drug just before a generic launches, then push patients to the new version. Or “pay-for-delay” deals, where brand-name makers pay generic companies to delay entering the market. The Actuarial Research Corporation estimates these practices cost the system $12 billion a year. Medicare alone loses $3 billion annually because of them.
And then there’s patent thickets - dozens of overlapping patents that block generics from entering for years. The Congressional Budget Office estimates ending these practices could save $1.8 billion over ten years. These aren’t just corporate tricks. They’re policies that keep prices high and savings low.
Generics Are Saving Medicare - But the System Is Under Threat
Medicare saved $142 billion in 2024 thanks to generics. That’s $2,643 per beneficiary. Imagine if every senior had to pay full price for their medications. Many couldn’t afford it. They’d skip doses. They’d end up in the hospital. Generics prevent that.
But the manufacturers making these drugs are struggling. The prices are so low now that some companies can’t make a profit. The Biosimilars Council warns that if this continues, manufacturers will shut down production. Drugs will disappear from shelves. Shortages will rise. We’ve already seen it happen with antibiotics, steroids, and even essential heart medications.
There’s a dangerous irony here: the system that saves billions is being starved of resources to keep running. Generic drugmakers need fair pricing to stay in business. They don’t need to charge like brand-name companies. But they do need to cover costs - for quality control, raw materials, and compliance. Right now, many are operating on razor-thin margins.
What’s Next? The Future of Generic Drug Savings
The Department of Health and Human Services is pushing a “Most-Favored-Nation” pricing model - meaning the U.S. would pay no more than the lowest price paid by other developed countries. Right now, Americans pay three to five times more for the same drugs than people in Canada, Germany, or Australia. If this policy takes hold, it could bring brand-name prices down - but it could also squeeze generic manufacturers further.
On the flip side, biosimilar adoption is only accelerating. More drugs are coming off patent. More alternatives are being approved. The FDA is streamlining reviews. By 2025, specialty drugs - which are mostly brand-name - will make up 60 percent of total drug spending, even though they’re prescribed in only a small fraction of cases. That means the pressure to use generics and biosimilars will only grow.
Here’s what’s clear: generics are not just a cost-cutting tool. They’re a lifeline. They keep people healthy. They keep hospitals from being overwhelmed. They keep insurance premiums from skyrocketing. But they can’t survive if we treat them like commodities instead of critical infrastructure.
What You Can Do
If you’re on a prescription, ask your doctor or pharmacist: “Is there a generic version?” If your insurance denies it, appeal. Many plans have tiered pricing - generics are often in the lowest tier. If you’re uninsured, check patient assistance programs. Many generic manufacturers offer discounts.
And if you’re someone who votes or contacts your representatives, push for policies that stop pay-for-delay deals, end product hopping, and crack down on patent abuse. These aren’t just corporate issues. They’re health issues. The $467 billion saved in 2024 didn’t happen by accident. It happened because generics were allowed to compete. Protect that competition. It’s the only thing keeping drug prices from exploding again.
Are generic drugs as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredients, strength, dosage form, and route of administration as the brand-name version. They must also meet the same strict standards for quality, purity, and performance. Studies consistently show no difference in effectiveness or safety between generics and brand-name drugs. The only differences are in inactive ingredients - like color or filler - which don’t affect how the drug works.
Why are generic drugs so much cheaper?
Generic manufacturers don’t have to repeat expensive clinical trials to prove safety and effectiveness. They only need to show their product is bioequivalent to the brand-name drug. That cuts development costs dramatically. Plus, once multiple companies start making the same generic, competition drives prices down. Brand-name companies, on the other hand, recoup R&D costs through high prices during their patent monopoly - which can last up to 20 years.
Do generic drugs have more side effects?
No. There is no evidence that generic drugs cause more side effects than brand-name drugs. The FDA monitors adverse events for both types of medications equally. Any differences in side effects reported are usually due to variations in inactive ingredients - like dyes or fillers - which can rarely cause allergic reactions. But these are uncommon and not unique to generics.
Why do some pharmacies charge more for generics?
Some pharmacies, especially independent ones, may charge more because they don’t have volume discounts or negotiate with pharmacy benefit managers (PBMs) as effectively as big chains. Also, some PBMs steer patients toward higher-priced generics if they get rebates from manufacturers. Always ask for the lowest cash price - sometimes paying out-of-pocket without insurance is cheaper than using your plan.
Can I trust generics if they look different from my brand-name drug?
Absolutely. The appearance - color, shape, size - of a generic drug doesn’t affect how it works. These differences are required by law to avoid trademark infringement. The active ingredient is identical. If you’re unsure, check the drug’s label or ask your pharmacist for the National Drug Code (NDC). It will confirm the generic matches the brand in strength and dosage.
What’s the difference between a biosimilar and a generic?
Generics are exact copies of small-molecule drugs - pills, capsules, liquids. Biosimilars are highly similar versions of complex biologic drugs - usually injected or infused, made from living cells. Because biologics are made from living organisms, biosimilars can’t be exact copies, but they’re proven to work the same way with no clinically meaningful differences. They’re not “generics,” but they serve the same purpose: lowering costs without sacrificing safety.
Final Thought: The Real Cost of Not Using Generics
Every time you choose a brand-name drug over a generic - without medical reason - you’re not just paying more. You’re contributing to a system that rewards price hikes over patient access. The $467 billion saved in 2024 didn’t come from magic. It came from competition, regulation, and millions of people choosing the cheaper, equally effective option. That system is working. But it’s fragile. Protect it. Ask for the generic. Push for fair policies. Your health - and your wallet - will thank you.


Written by Felix Greendale
View all posts by: Felix Greendale