What Is Hepatic Encephalopathy?
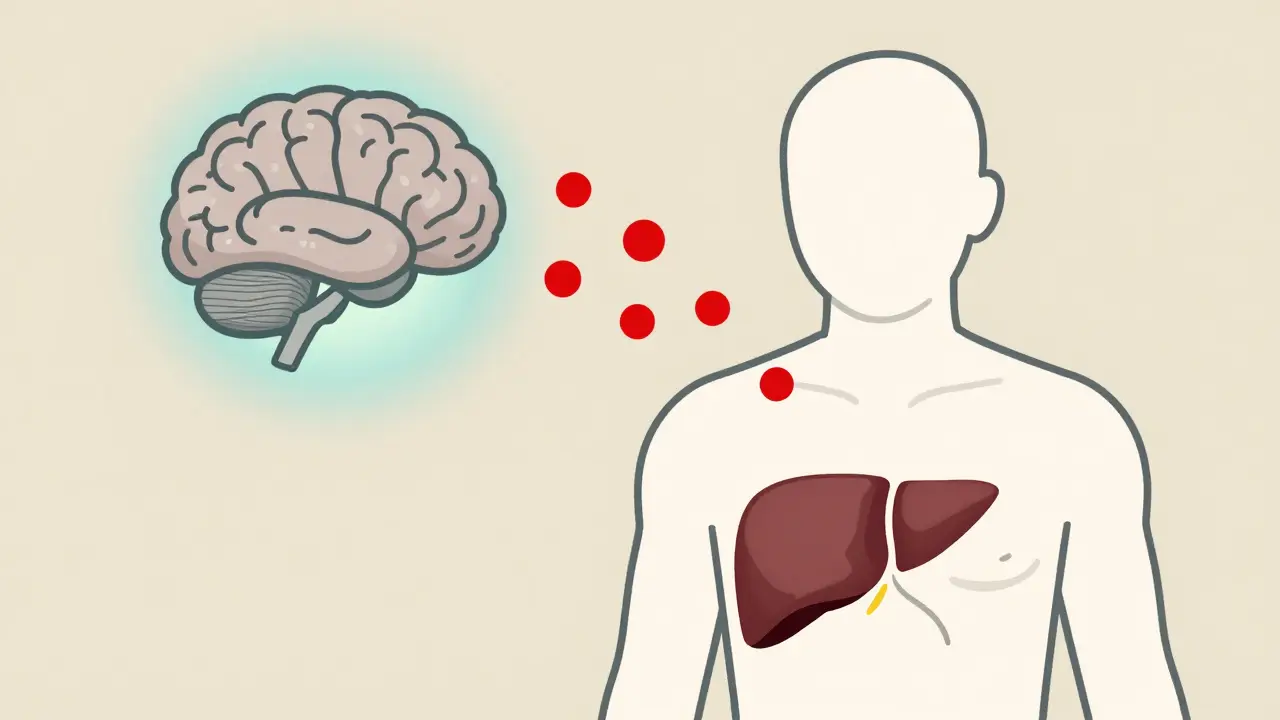
When your liver can't clean your blood properly, toxins like ammonia build up and start affecting your brain. This isn't just fatigue or memory lapses-it's a real neurological condition called hepatic encephalopathy (HE). It happens mostly in people with advanced liver disease, especially cirrhosis. About 30 to 45% of those with cirrhosis will develop noticeable symptoms at some point. Even more-up to 80%-have subtle brain changes that only show up on special tests.
HE doesn't come on suddenly like a stroke. It creeps in. At first, you might just feel a little off-sleeping more than usual, forgetting names, or having trouble focusing. These are called minimal HE. Then it can get worse: confusion, personality shifts, slurred speech, even coma. The main culprit? Ammonia. Your gut makes it when bacteria break down protein. A healthy liver filters it out. But when the liver is damaged, ammonia slips through and reaches the brain, causing swelling and messing with nerve signals.
Why Lactulose Is the First-Line Treatment
Since the 1960s, lactulose has been the go-to medicine for HE. It's not a cure, but it works. And it's cheap-generic versions cost $15 to $30 a month. Lactulose is a sugar your body can't digest. Instead, it travels to your colon, where gut bacteria break it down. This creates an acidic environment, turning ammonia (NH₃) into ammonium (NH₄⁺), which can't cross into your bloodstream. At the same time, it pulls water into your bowels, making you poop more. That's how it gets rid of ammonia-through your stool.
Doctors usually start with 30 to 45 mL three or four times a day, taken by mouth. The goal? Two to three soft bowel movements daily. Too little, and it won't help. Too much, and you'll be in the bathroom all day. That's why dosing is personal. If you're not having enough stools after 48 hours, your dose needs to go up. A University of Michigan study found that 65% of people who didn't respond to lactulose were actually getting too little-sometimes less than 30 mL a day.
Some people can't take it orally. In those cases, doctors use a lactulose enema: 300 mL mixed with 700 mL water, given rectally. It works faster. In emergency situations, like when someone is heading toward coma, this can be life-saving.
What Happens When Lactulose Isn't Enough?
One in five people with HE don't get better with lactulose alone. That's where rifaximin comes in. Approved by the FDA in 2010, this antibiotic doesn't get absorbed into your blood-it stays in your gut. It kills the bad bacteria that make ammonia, especially Klebsiella and Proteus. Studies show it cuts down on HE flare-ups by 58% compared to placebo. Most doctors now add it to lactulose for people who've had more than one episode. The standard dose is 550 mg twice a day.
But it's expensive-around $1,200 a month. That's why it's not the first step. It's for maintenance. Also, there's a small risk: about 0.2% of people develop C. diff infection from long-term use. Still, for many, the trade-off is worth it. One patient on a liver forum said, "After six months of lactulose and rifaximin, my cognitive test scores improved and I went back to part-time work."

What Triggers a Hepatic Encephalopathy Episode?
HE doesn't just happen out of nowhere. Something usually sets it off. The most common triggers? Infections, bleeding, and electrolyte problems. Spontaneous bacterial peritonitis-an infection in the belly fluid-causes 25 to 30% of flare-ups. Upper GI bleeding from varices is next, at 20 to 25%. Then there's low potassium, dehydration, or too much protein. Even constipation can make it worse because ammonia sits in your colon longer.
Many people don't realize how sensitive their brain is to these changes. One caregiver on Reddit tracked her husband's episodes for months and noticed every time he got a urinary tract infection (UTI), he became confused. After starting monthly UTI tests, they prevented 80% of his HE flares. That’s the kind of insight that saves lives.
Doctors also warn against certain drugs. Benzodiazepines-like Valium or Xanax-can make HE 3.2 times worse. Even over-the-counter sleep aids can be dangerous. Always check with your liver specialist before taking anything new.
How to Prevent Hepatic Encephalopathy
Prevention is way better than treatment. For people with cirrhosis who've had HE before, doctors often prescribe low-dose lactulose daily-15 mL twice a day. This simple step cuts recurrence by half within six months. It’s not just about medicine. Diet matters too. You don’t need to cut protein completely. In fact, eating too little can make you weaker. The goal is 1.2 to 1.5 grams of protein per kilogram of body weight daily. That’s about 80 to 100 grams for a 150-pound person. Focus on plant-based and dairy proteins-they’re easier on the liver than red meat.
Stay hydrated. Watch for signs of infection. Get vaccinated for hepatitis A and B, flu, and pneumonia. Get regular checkups. And if you live alone, make sure someone knows your symptoms. Family members spot HE 48 to 72 hours before doctors do in 65% of cases. A simple tool called the EncephalApp Stroop test is free on your phone. It takes five minutes and can catch early changes.
When to Seek Help Immediately
Not all confusion is HE. But if you have liver disease and suddenly feel disoriented, can't remember your name, or start speaking incoherently, don't wait. Go to the ER. About 15 to 20% of HE cases require ICU care because the person is at risk of stopping breathing. Mortality in those cases is 25 to 30%. The sooner you treat it, the better the chance of full recovery.
Even if you're not in crisis, if your lactulose isn't working after two days, call your doctor. Your dose might need adjusting. Or there could be a hidden trigger-like a hidden infection or kidney issue-that needs fixing.
What’s Next for Hepatic Encephalopathy Treatment?
The field is changing fast. Researchers are looking beyond ammonia. The gut-brain axis is now a major focus. Fecal microbiota transplants (FMT)-basically, poop from a healthy donor-have helped 70% of patients with stubborn HE in early trials. A new oral adsorbent called AST-120, already used in Japan, is now approved in Europe. It binds toxins in the gut before they’re absorbed.
There’s also a new FDA-approved combo pill called Xifaxilac, which mixes lactulose and rifaximin into one tablet. And in 2023, the NIH launched a $5.2 million project to develop a blood test that can predict HE risk with 85% accuracy using 12 biomarkers. Soon, you might not wait for symptoms-you’ll get warned before they start.
Real-Life Challenges: Adherence and Stigma
Here’s the hard truth: most people don’t stick with treatment. Only 52% of patients take their lactulose correctly after six months. Why? The taste is awful. The diarrhea is embarrassing. One patient said, "It saved me from the hospital, but the constant bathroom trips ruined my job interviews."
And there’s stigma. Many people with HE are misdiagnosed as having dementia. A British Liver Trust survey found 31% were told they had Alzheimer’s before anyone thought of liver disease. That delay costs time-and brain function. Social isolation is common. 42% of patients say they stopped seeing friends because they feared having a confusing episode in public.
But it doesn’t have to be this way. With the right support, education, and consistent treatment, people with HE can live full lives. Many return to work. Many stay out of the hospital. The key is catching it early, treating it right, and not giving up.

Written by Felix Greendale
View all posts by: Felix Greendale