Every year, thousands of patients in hospitals and clinics are harmed-not by their illness, but by a simple mistake with a pill, an injection, or an IV drip. Most of these errors are preventable. And one of the most powerful tools to stop them? A second set of eyes.
What Makes a Medication High-Risk?
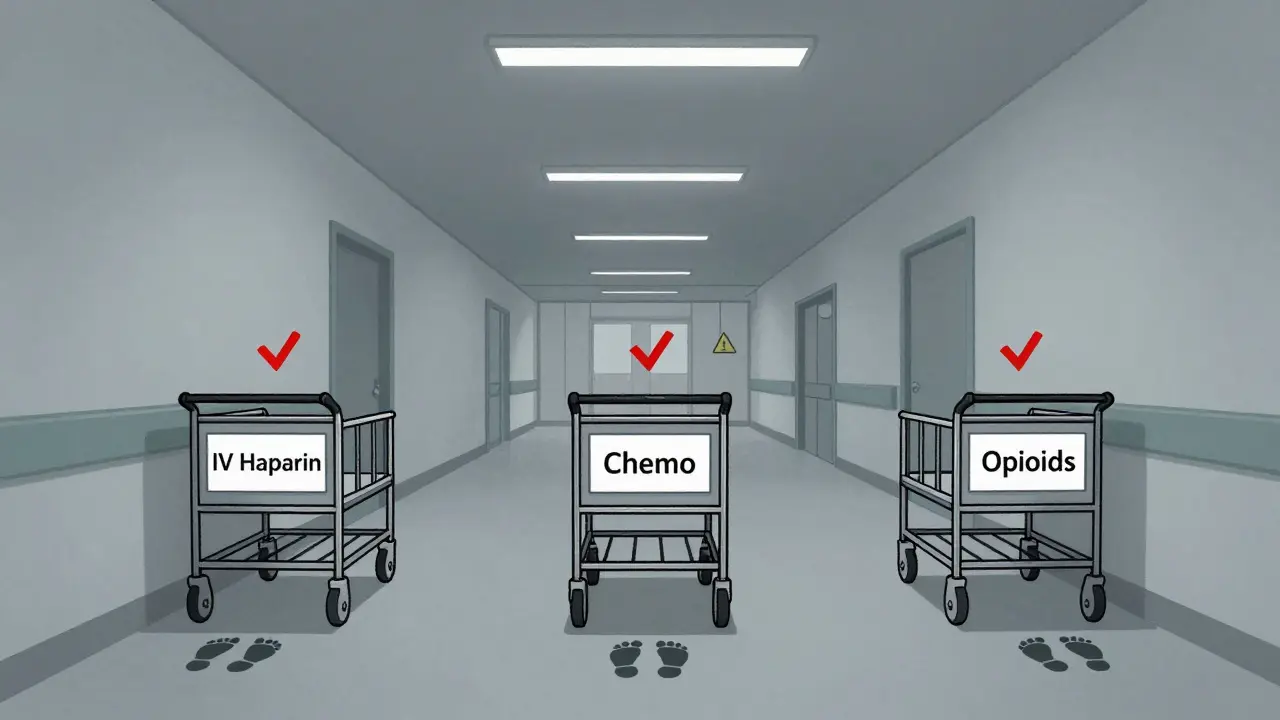
Not all medications are created equal when it comes to danger. Some drugs, even in tiny mistakes, can kill. These are called high-risk medications. They’re not rare. In fact, you’ll find them in nearly every hospital ward, ICU, and cancer center. But because they’re so dangerous, they demand more than just a quick check. They need a full, independent double verification before they’re given to a patient. The Institute for Safe Medication Practices (ISMP) defines these as drugs with a heightened risk of causing significant patient harm when used incorrectly. That means even a 10% dosing error can turn a life-saving treatment into a fatal one. Think of it like driving a car with no brakes. You wouldn’t trust yourself to stop it without a backup. The same logic applies here. The most common high-risk medications include:- IV insulin
- IV heparin (a blood thinner)
- Concentrated potassium chloride
- IV opioids like morphine or fentanyl
- Chemotherapy drugs
- Cardiovascular drugs like sodium nitroprusside or epinephrine
Why Double Checks Are Non-Negotiable
A single nurse checking a medication is a good start. But it’s not enough. Human error is inevitable. We get tired. We’re interrupted. We assume the label says what we think it says. That’s why the standard now requires two qualified professionals to independently verify the medication before it’s given. This isn’t just a policy. It’s a legal requirement under The Joint Commission’s Standard MM.05.01.09, effective January 1, 2023. Every healthcare facility must have a written list of their high-risk medications and a clear process for verifying them. The double check isn’t just two people glancing at the same thing. It’s a true independent verification. That means:- The second person doesn’t watch the first person do their check.
- Both calculate the dose separately.
- Both confirm the patient’s name, date of birth, and medical record number.
- Both verify the drug name, strength, route, and expiration date.
- Both sign the Medication Administration Record (MAR) to prove it happened.
Where Double Checks Are Required
The exact list of medications requiring double checks varies by hospital, but most follow the ISMP’s 2022 guidelines. Here’s what’s commonly mandated:- IV insulin: Even a 0.1 mL error can cause severe hypoglycemia. Double check required before every dose.
- IV heparin: Too much = internal bleeding. Too little = blood clots. Both are deadly.
- Chemotherapy: These drugs are toxic by design. A wrong dose can kill healthy cells. Two oncology nurses must verify the drug, dose, patient, and infusion rate before starting.
- IV opioids: Especially epidural or intrathecal forms. A single misplaced dose can stop breathing.
- Concentrated potassium chloride: One vial of this can kill if given too fast. It’s stored in locked cabinets and requires two people to retrieve and verify.

The Reality: Double Checks Are Often Skipped
Here’s the uncomfortable truth: double checks aren’t always done. A 2022 ISMP survey found that 68% of nurses admitted skipping required double checks during busy shifts. Why? Lack of time. Lack of staff. Pressure to move patients through the system. And sometimes, just plain fatigue. One nurse in a busy urban hospital told me: “I’ve done 30 insulin checks this shift. I’m exhausted. I know I’m supposed to get a second person, but the charge nurse is on the phone with a family member, and the patient’s family is waiting for the next dose. I do it myself and write it down. I’m not proud of it.” That’s the problem. When double checks become a checkbox instead of a safety net, they lose their power. And that’s when errors happen.Technology Is Changing the Game
Barcode scanning at the bedside is now a game-changer. When a nurse scans the patient’s wristband and the medication’s barcode, the system checks: Is this the right drug? Is this the right dose? Is this the right time? If something’s wrong, it alerts the nurse before the drug is even opened. The ECRI Institute says barcode scanning is more reliable than manual double checks for catching these errors. It doesn’t get tired. It doesn’t assume. It doesn’t miss a decimal point. But technology isn’t perfect. It can’t catch errors in how a drug is prepared-like mixing the wrong concentration of insulin or misprogramming an infusion pump. That’s where human judgment still matters. That’s why the smartest hospitals now use a hybrid approach:- Use barcode scanning for routine verification.
- Reserve manual double checks for the highest-risk scenarios: chemotherapy, IV opioids, concentrated electrolytes.
What You Can Do: A Simple Safety Checklist
Whether you’re a nurse, pharmacist, or patient advocate, here’s what you can do to help prevent errors:- Always ask: “Is this a high-risk medication?” If yes, insist on a double check.
- Never let someone else do the math for you. Do your own calculation.
- Verify the patient’s name and DOB with them, not just the wristband.
- If you’re the second checker, don’t just nod along. Look at the original order, the label, and the vial yourself.
- If you’re pressured to skip a check, speak up. Your silence could cost a life.
The Future: Fewer Checks, But Better Ones
The old way was to double-check everything. The new way is to double-check only what matters. ISMP now says: “Fewer independent double checks, strategically placed at the most vulnerable points, will be much more effective than an overabundance.” That means:- Stop requiring double checks for low-risk drugs like oral antibiotics.
- Focus on IV insulin, heparin, opioids, and chemo.
- Use technology to handle the routine stuff.
- Train staff not just on how to check, but why it matters.
What are the most dangerous medications that require a double check?
The most dangerous medications requiring double verification include IV insulin, IV heparin, concentrated potassium chloride, IV opioids (especially epidural or intrathecal), and chemotherapy drugs. These can cause death or severe harm even with small dosing errors. Hospitals follow ISMP guidelines to identify which drugs on their formulary require this extra step.
Who can perform a double check?
Only qualified healthcare professionals can perform a double check. This includes registered nurses, pharmacists, and prescribers (doctors, nurse practitioners, physician assistants). The second person must be trained and authorized to verify medications. In some settings, only nurses are allowed to witness controlled substance checks.
Can a pharmacist and nurse do the double check together?
Yes, a pharmacist and nurse can perform a double check together, but they must do it independently. The pharmacist verifies the prescription and preparation, while the nurse confirms the patient, route, and timing. Neither should see the other’s work until both have completed their own checks. This prevents confirmation bias.
Are double checks always effective?
No. Studies show that double checks can fail if they’re rushed, poorly trained, or done without true independence. Nurses often skip them during busy shifts. The key is not to do more checks-but to do them right. Focus on the highest-risk drugs and use technology like barcode scanning to support, not replace, human judgment.
What happens if a double check is skipped?
Skipping a double check is a serious breach of safety protocol. It can lead to patient harm, disciplinary action, and even legal consequences. Hospitals track these incidents through incident reporting systems. Repeated violations may result in mandatory retraining, suspension, or loss of privileges. The goal isn’t punishment-it’s prevention.


Written by Felix Greendale
View all posts by: Felix Greendale