When a drug gets recalled, it’s not just a press release or a notice on a website. It’s a life-or-death alert that lands directly in your pharmacy’s inbox-and if you miss it, someone could get hurt. Every year, thousands of medications are pulled from shelves because of contamination, mislabeling, or dangerous impurities. In 2023 alone, the FDA issued over 4,200 drug recalls. Most were Class II-potentially harmful but not immediately life-threatening-but 4% were Class I, meaning they could cause serious injury or death. Pharmacy-level recall notifications are your first and most critical line of defense. If you work in a pharmacy, you need to know exactly how to find, verify, and act on these alerts before a patient takes a bad pill.
Understand the Three Levels of Drug Recalls
Not all recalls are the same. The FDA classifies them into three categories, and each one demands a different response time and level of urgency.- Class I: The most serious. These drugs could cause serious health problems or death. Examples include pills with lethal contamination like elevated levels of NDMA (a known carcinogen) or insulin with incorrect dosing. Response time: 24 hours to verify and remove from inventory.
- Class II: May cause temporary or reversible health issues. Think pills with wrong labels, missing ingredients, or packaging defects that could lead to dosing errors. Response time: 72 hours to verify and notify patients.
- Class III: Unlikely to cause harm, but violate FDA labeling or manufacturing rules. These might be expired dates printed wrong or minor packaging flaws. Response time: 14 days to document and remove.
Knowing the class tells you how fast you need to move. A Class I recall in your inventory means you have less than a day to find every bottle, pull it from shelves, and contact every patient who received it. Waiting until the next morning isn’t an option.
Set Up Your Primary Notification Channels
You can’t rely on one source. The FDA, wholesalers, and manufacturers all send alerts-and they don’t always agree. You need at least three ways to get notified.- FDA MedWatch Email Alerts: Free, official, and mandatory. Register at www.fda.gov/Safety/MedWatch and choose alerts for drug recalls. These come out weekly on Wednesdays, but Class I alerts can arrive anytime. Don’t skip this. It’s the only source that covers every recall nationwide.
- Your Wholesaler’s Recall System: If you buy from McKesson, Cardinal Health, or AmerisourceBergen, you’re already enrolled in their recall notification system. These are usually free and sent via email or integrated into your ordering portal. But here’s the catch: they often send false positives. One pharmacy tech told us they got 17 recall alerts last week-but only 3 actually applied to their inventory.
- Your Pharmacy Management System: This is your secret weapon. Systems like QS/1, PioneerRx, and FrameworkLTC pull FDA data hourly and cross-reference it with your inventory. If a recalled lot number matches a bottle in your stock, the system flags it automatically. No manual search needed. If your system doesn’t do this, you’re doing the work of 10 people.
Independent pharmacies often skip the automated system because of cost. But here’s the math: if you spend 3.2 hours a week manually checking recalls (as the NCPA found), and you pay $2,500 a year for a system like PioneerRx, you’re saving over 160 hours a year. That’s four full workweeks. That time is worth more than the subscription.
Verify the Recall With Exact Details
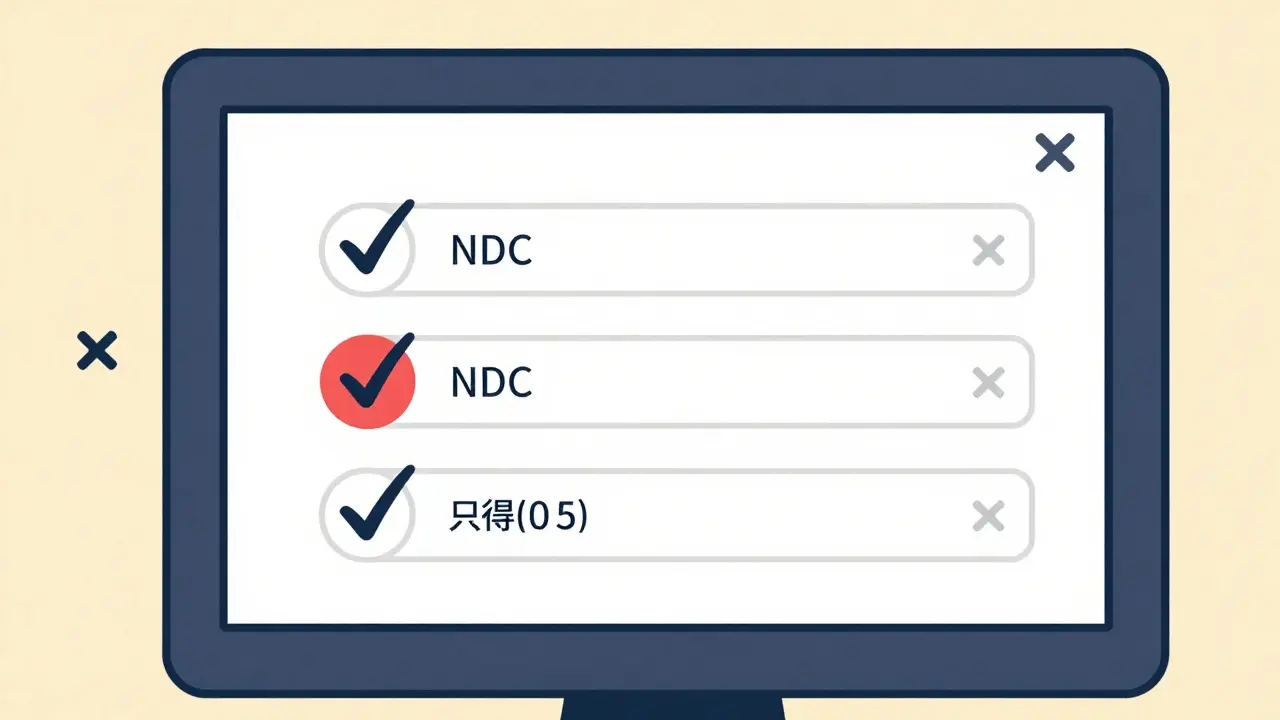
When you get a notice, don’t just assume it’s yours. You need to match three things: the National Drug Code (NDC), the lot number, and the expiration date.Here’s how to do it right:
- Find the exact NDC on the recall notice. It’s a 10- or 11-digit number that identifies the drug, manufacturer, and package size. Example: 00078-0212-01.
- Check your inventory for that exact NDC. Don’t rely on the drug name-different manufacturers use the same name. Your system should show you every bottle with that NDC.
- Match the lot number. This is where most mistakes happen. Lot numbers can look similar: “L231104” vs. “L231104A.” One letter changes everything. If your system doesn’t auto-match lots, you’re manually checking every bottle.
- Confirm the expiration date. Some recalls only affect specific batches with early expiration dates. If your bottle expires in 2027 and the recall is for 2024, you’re safe.
Pro tip: If the recall notice doesn’t list an NDC or lot number, call the manufacturer. The FDA requires them to provide it within 24 hours. If they don’t, report it. A vague recall notice is a red flag.
Act Fast-But Only on What’s Yours
Once you’ve confirmed the recall applies to your inventory, you have to act. But don’t panic and pull everything. Only remove the exact bottles that match.Here’s the protocol:
- Class I: Quarantine the product immediately. Lock it in a separate bin. Call every patient who received it in the last 6 months. You must notify 100% of them within 8 hours. Use your pharmacy system to pull dispensing records. If you don’t have that feature, you’re stuck calling patients one by one-good luck.
- Class II: Remove from shelves. Notify patients who received it in the last 3 months. You need to reach 80%. Leave a voicemail, send a text, or mail a letter. Don’t wait.
- Class III: Remove from inventory. Document the action. No patient notification needed unless the FDA says so.
And don’t forget: you must keep records for 3 years. That means printing or saving every email, every patient notification log, every inventory report. Electronic audit trails are now required by the FDA. Paper logs? They’re not enough anymore.
Fix the Gaps in Your System
Most pharmacies still operate like it’s 2015. They get emails, print them out, and stick them on a bulletin board. That’s not safe.Here’s what’s broken-and how to fix it:
- False positives: Your wholesaler sends 15 alerts, but only 2 matter. Solution: Use your pharmacy system to auto-filter. If it doesn’t cross-reference your inventory, upgrade.
- No after-hours access: A recall hits at 8 p.m. on a Saturday. Your tech can’t log in to check inventory. Solution: Make sure your system is cloud-based and accessible from phones. Many systems now have mobile apps.
- Missed sync patients: A patient gets a 90-day supply. The recall is for a pill they got 60 days ago. You don’t know they still have it. Solution: Ask your system to flag patients on multi-month prescriptions. The FDA requires this by 2025. Start now.
- Staff overwhelmed: One pharmacist told us they missed a recall because they were busy with insurance calls. Solution: Assign a recall coordinator. It’s one person’s job-just like infection control or OSHA compliance. Train them. Pay them extra. It’s worth it.

What’s Coming in 2025 and Beyond
The system is changing fast. By January 2025, every Class I recall notice must include patient-level risk data. That means the FDA will start telling you exactly who received the bad drug-based on pharmacy dispensing records. You won’t have to guess anymore.By 2027, AI-powered systems will auto-verify recalls in under 5 minutes. They’ll cross-check your inventory, patient records, and recall data in real time. No human input needed. The University of Pittsburgh estimates this will cut patient exposure to recalled drugs by 82%.
Right now, only 89% of hospital pharmacies use these systems. Only 31% of independent pharmacies do. If you’re still using paper logs or Excel sheets, you’re not just behind-you’re at risk.
What to Do Right Now
If you read this and realized you’re not doing enough, here’s your 5-minute action plan:- Go to www.fda.gov/Safety/MedWatch and sign up for email alerts. It takes 2 minutes.
- Ask your pharmacy system vendor: “Do you auto-match FDA recall lots with our inventory?” If they say no, ask for a demo of a system that does.
- Assign one person to check recall alerts every morning. Even if it’s just 10 minutes.
- Print out your top 5 most dispensed drugs. Check their NDCs against the latest FDA recall list. Do any match? If yes, act now.
- Start keeping digital records of every recall you handle. Save emails, patient notifications, and inventory reports. You’ll need them.
Drug recalls aren’t going away. They’re getting more frequent. In 2023, nitrosamine impurities caused over 40% of recalls. That number will rise. The only way to protect your patients-and your pharmacy-is to be ready before the next alert hits.


Written by Felix Greendale
View all posts by: Felix Greendale