When You Need to Take Medication but Still Want to Keep Breastfeeding
It’s common to need a short course of antibiotics, painkillers, or other meds while breastfeeding. Maybe you’ve got a sinus infection, a sprained ankle, or a postpartum headache. The last thing you want is to stop nursing your baby. The good news? Most medications are safe to take while breastfeeding, and you don’t need to throw away your milk. But you do need to store and label it right.
Too many moms panic and dump their milk because they’re unsure. A 2023 survey of over 300 breastfeeding mothers found that 41% threw out milk they didn’t need to-just because they weren’t sure what to do. You don’t have to be one of them.
Do You Really Need to Pump and Dump?
The short answer? Almost never.
Less than 2% of all medications require you to stop breastfeeding, even temporarily. That’s according to Dr. Thomas Hale’s Medications and Mothers’ Milk, the most trusted reference in lactation medicine. Most drugs pass into breast milk in tiny amounts-far less than what your baby would get from a direct prescription. Your body naturally clears the medication over time. The key isn’t dumping milk. It’s timing.
For example, if you take ibuprofen after a feed, your milk will have the lowest amount of the drug right before your next feed. That’s when you want to nurse. Same with amoxicillin, acetaminophen, or most antidepressants. No need to pump and dump. Just nurse as usual.
There are exceptions. Some medications used for cancer, radiation, or severe psychiatric conditions might require a short pause. But your doctor or lactation consultant will tell you if you’re one of the rare cases. Don’t assume. Ask.
Labeling Your Milk Like a Pro
If you’re taking medication, your milk isn’t all the same. You need to separate it.
Every container of breast milk should have:
- The date and time you pumped
- Your baby’s name
- The name of the medication
- The dose you took
- The time you took it
Use waterproof labels and permanent ink. Stick-on labels work best. Don’t write directly on the bag with a marker-it smudges. If you’re using a hard container, use masking tape and a fine-tip pen.
Why all this detail? Because different batches of milk have different drug levels. Milk pumped right after you take a pill? That’s the highest concentration. Milk pumped 4-6 hours later? Much lower. You need to know which is which.
How to Store Medication-Affected Milk
Storage rules stay the same, but you need to keep affected milk separate.
Here’s the standard timeline:
- Room temperature (up to 25°C): 4 hours max
- Refrigerator (4°C or colder): 4 days max
- Freezer (0°C or colder): 6-12 months
But here’s the catch: if you’re on a short-term med (like a 5-day antibiotic), you should store milk in batches based on when you took the dose.
For example:
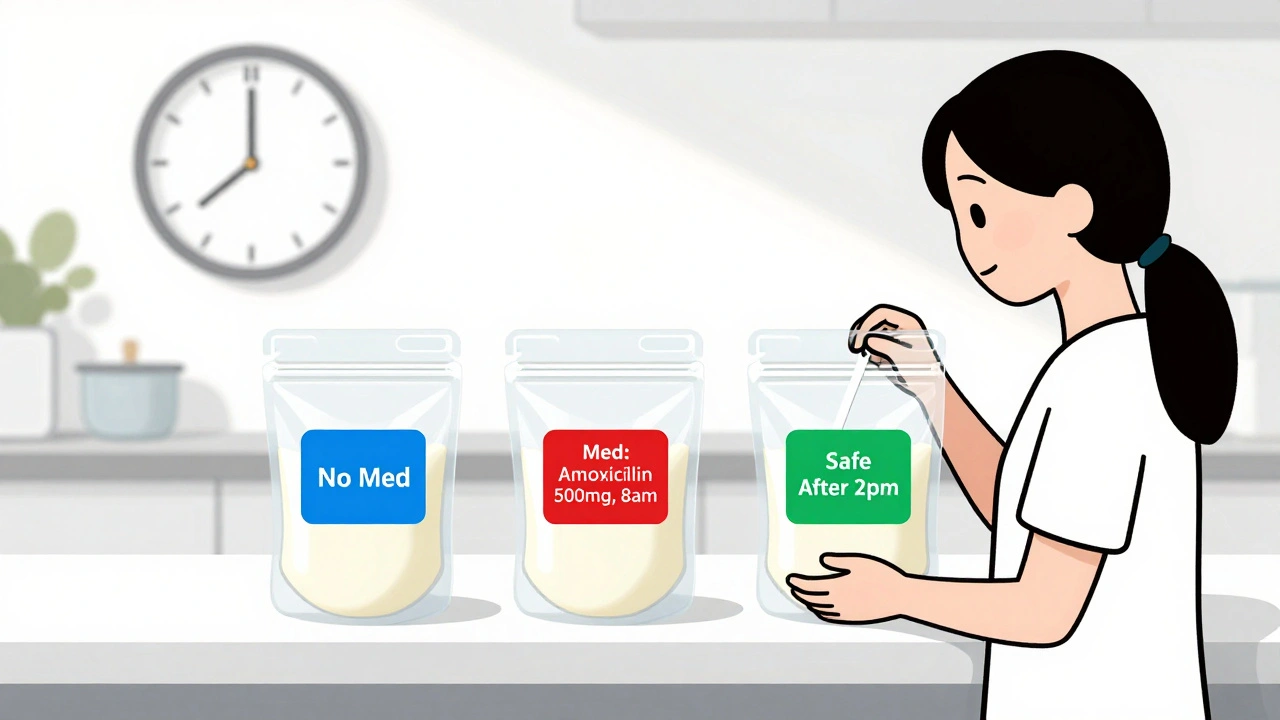
- Batch 1: Milk pumped before you started the med → labeled “No Med”
- Batch 2: Milk pumped 1 hour after your first pill → labeled “Med: Amoxicillin 500mg, 8am”
- Batch 3: Milk pumped 6 hours after your first pill → labeled “Med: Amoxicillin 500mg, 2pm”
Store each batch in a separate bag or container. Use different colored labels or stickers to make it easy. Blue for “before med,” red for “after med,” green for “safe again.”
Why? Because your baby might be fine with milk from Batch 3, but you don’t want to accidentally feed them milk from Batch 2 if you’re unsure.

What About Freezing?
Freezing is your best friend here. It stops the milk from spoiling and lets you wait until the medication clears.
Always leave an inch of space at the top of the container. Milk expands when it freezes. If you fill it to the brim, the bag might burst in the freezer.
Store your labeled batches in the back of the freezer, where the temperature is most stable. Don’t put them near the door. Every time you open it, the temp changes.
When you’re ready to use it, thaw the oldest batch first. Use the “first in, first out” rule. If you’re unsure about a batch, check the label. If it says “Med: 2pm,” and you took the last pill at 8am, and the drug has a 4-hour half-life, then 6 hours later, it’s likely safe.
What If You’re Traveling?
Carrying milk with you while on meds? No problem.
Use an insulated cooler bag with frozen ice packs. The CDC says this keeps milk safe for up to 24 hours. Put the bags in a sealed plastic container inside the cooler to prevent leaks. Keep it with you, not in checked luggage.
If you’re flying, bring a doctor’s note explaining you’re transporting breast milk. TSA allows it through security without limits. You don’t need to taste it or open it. Just say, “It’s breast milk,” and they’ll let you through.
When Can You Start Using the Stored Milk Again?
This is where most moms get stuck.
Most medications clear from your system in 2-4 half-lives. A half-life is how long it takes for half the drug to leave your body.
For common meds:
- Amoxicillin: Half-life = 1 hour → safe after 4-6 hours
- Ibuprofen: Half-life = 2 hours → safe after 8-12 hours
- Paracetamol (acetaminophen): Half-life = 2-3 hours → safe after 8-12 hours
- Propranolol: Half-life = 4 hours → safe after 16-24 hours
So if you took a pill at 8am, and it’s now 8pm? That’s 12 hours. For most meds, that’s plenty of time. Check the label on your milk. If it says “Med: 8am,” and it’s now 8pm, you’re good to use it.
Still unsure? Use the MotherToBaby app (updated 2024). It lets you enter your medication and tells you exactly when your milk is safe. Or call your local lactation consultant. They’ve seen this a hundred times.

What to Avoid
Here are the top mistakes moms make:
- Mixing affected milk with clean milk. Don’t do it. You risk feeding your baby a higher dose than intended.
- Labeling only the date. Without the med name and time, you’re guessing. That’s dangerous.
- Throwing away milk too soon. Most moms waste 30-50% more milk than needed because they’re scared.
- Assuming all meds are the same. A cold pill isn’t the same as an antibiotic. Each one acts differently.
One mom I spoke to in Brighton dumped 12 liters of milk during her 10-day antibiotic course. She didn’t know the drug was safe. She could’ve used 90% of it. She cried when she found out.
What to Do If You’re Still Worried
If you’re unsure, don’t guess. Don’t rely on Reddit or Facebook groups. Those aren’t medical advice.
Instead:
- Ask your pharmacist. They’re trained in drug transfer into breast milk.
- Call your IBCLC (International Board Certified Lactation Consultant).
- Use the LactMed database (free, from the NIH). Just search your drug name.
- Ask your doctor: “Is this safe for breastfeeding? Do I need to pump and dump?”
If your prescription doesn’t say anything about breastfeeding, ask for a printed handout. Most pharmacies now give them. If they don’t, ask for a referral to a lactation specialist.
You’ve Got This
Taking medication doesn’t mean you have to stop breastfeeding. It just means you need to be a little more organized. Label clearly. Store separately. Wait a few hours. And trust the science.
Over 89% of moms who followed proper labeling and storage guidelines were able to safely use 75-100% of their stored milk after medication use, according to the Lactation Network. You can be one of them.
Don’t let fear make you waste milk. Your baby needs your milk. And you’ve got the power to keep giving it to them-safely.
Do I need to pump and dump if I take a one-time painkiller?
No. For most one-time painkillers like ibuprofen or acetaminophen, you don’t need to pump and dump. Wait 2-4 hours after taking the dose, then nurse. The amount that passes into your milk is tiny and won’t harm your baby. Pumping and dumping won’t make it safer-it just wastes your milk.
Can I freeze milk I pumped before I started my medication?
Yes, and you should. Milk pumped before you started your medication is completely safe and doesn’t need special labeling beyond the date and your baby’s name. Keep it separate from milk pumped during your treatment. Use this first when you’re done with the meds.
What if I accidentally mix medicated milk with clean milk?
If you mixed a small amount of medicated milk with a large batch of clean milk, it’s likely still safe-especially if the medication is low-risk. But if you’re unsure, don’t feed it. Save it for later and consult your lactation consultant. In the future, always use separate containers and label clearly to avoid this.
How long should I wait after taking a medication before pumping?
Wait at least 2-4 hours after taking your dose. That’s usually enough time for the drug levels in your milk to drop. If you’re on a medication with a long half-life (like some antidepressants), your provider may suggest waiting longer. Always check the specific guidance for your drug.
Is it safe to use milk that’s been in the fridge for 5 days while I was on meds?
No. Even without medication, breast milk should be used within 4 days when refrigerated. After that, bacterial growth increases, even if it doesn’t smell bad. If you’ve had milk in the fridge for 5 days, discard it. Don’t risk your baby’s health.
Can I use a smartphone app to help me track my milk and meds?
Yes. Apps like MotherToBaby (updated 2024) let you enter your medication and generate a custom label with safe pumping windows. They also tell you when your milk is safe to use again. These tools are backed by medical research and used by lactation consultants.
What if I’m taking antibiotics for a long time?
Most antibiotics are safe for long-term use while breastfeeding. You still don’t need to pump and dump. Just keep labeling your milk by dose time. If you’re on antibiotics for more than 10 days, talk to your doctor about whether you need a different one. Some can affect your baby’s gut bacteria, but that’s rare.
Do I need to label the milk if I’m only on a 1-day medication?
Yes. Even if it’s just one dose, label it. You might forget what you took or when. And if you pump more than once that day, you could have different batches. Labeling takes 10 seconds. It saves you from confusion-and wasted milk-later.

Written by Felix Greendale
View all posts by: Felix Greendale