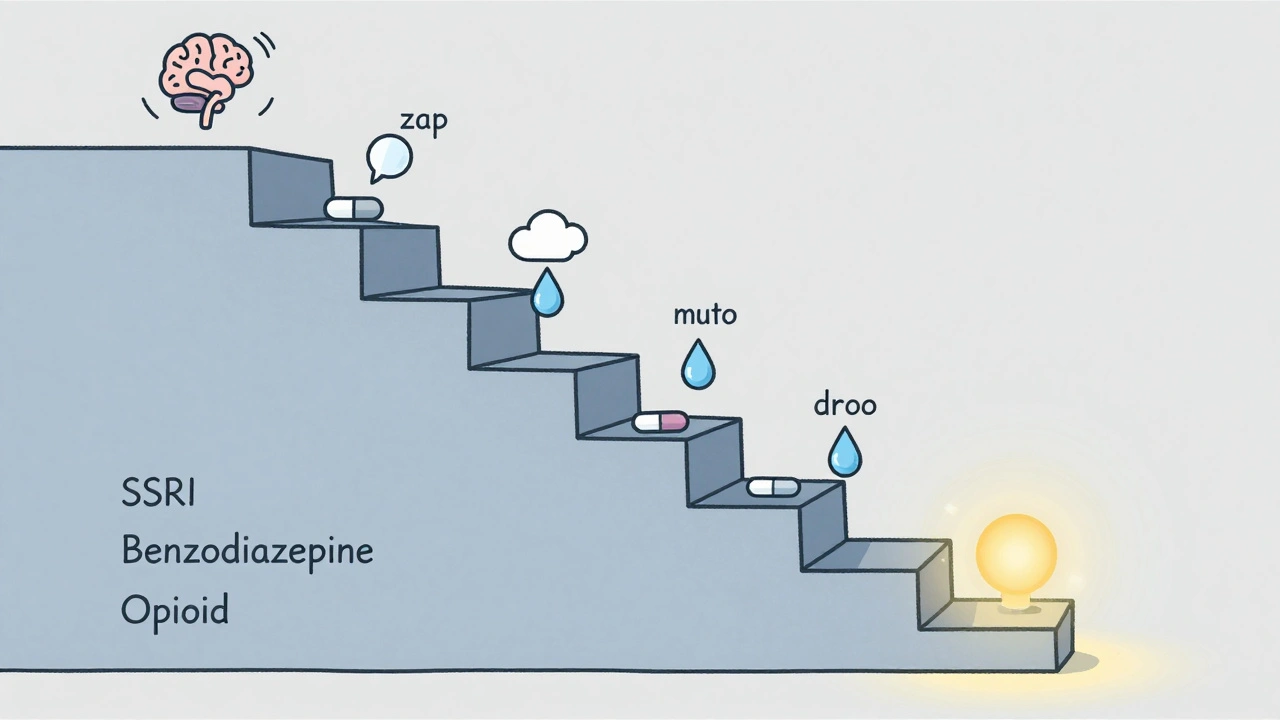
Stopping a medication isn’t like turning off a light switch. For many people, especially those on long-term prescriptions for antidepressants, benzodiazepines, or opioids, suddenly stopping can trigger a cascade of uncomfortable - or even dangerous - symptoms. Anxiety, insomnia, dizziness, nausea, electric-shock sensations, and in rare cases, seizures or suicidal thoughts can follow abrupt discontinuation. But here’s the truth: most of these risks can be avoided with the right conversation and a carefully planned taper. The key isn’t just knowing when to stop - it’s knowing how to talk about it with your provider.
Why Tapering Isn’t Optional for Some Medications
Not every medication needs a slow taper. But for drugs that affect your brain chemistry - like SSRIs (sertraline, escitalopram), benzodiazepines (alprazolam, clonazepam), or opioids (oxycodone, tramadol) - your body adapts. Over weeks or months, your nervous system rewires itself to function with the drug present. Take it away too fast, and your brain scrambles to catch up. That’s withdrawal. According to the American Society of Addiction Medicine, 8-12% of people on long-term benzodiazepines experience severe withdrawal. For antidepressants, up to 71% of clinical guidelines recommend gradual tapering. The CDC estimates that 17,000 deaths each year are linked to improper opioid discontinuation. These aren’t rare edge cases. They’re predictable outcomes of poor communication. The goal of tapering isn’t to make you feel worse longer - it’s to make the transition smooth enough that you don’t feel the need to go back. Studies show that structured tapers have a 78% completion rate. Unstructured ones? Just 42%.What Your Provider Needs to Know Before Starting
Before you even mention tapering, prepare. Bring your full medication list - including over-the-counter drugs, supplements, and alcohol use. Many people don’t realize that even something like St. John’s Wort or high-dose ibuprofen can interact with tapering. Your provider should ask you:- Why do you want to stop? (Side effects? Fear of dependence? Feeling better?)
- How has this medication affected your daily life - sleep, mood, energy, work?
- Have you had withdrawal symptoms before?
- Are you under stress right now? (Divorce, job loss, illness - these make tapering harder.)
How to Ask for a Taper Without Feeling Guilty
Many patients stay on meds longer than they want because they’re afraid of sounding ungrateful. You’re not. You’re managing your health. Try phrases like:- “I’ve been feeling better, and I’d like to see if I can reduce this medication. Can we talk about a plan?”
- “I’m worried about long-term use. What would a safe taper look like for me?”
- “I read that stopping suddenly can cause withdrawal. Can we avoid that?”
What a Realistic Taper Plan Looks Like
There’s no one-size-fits-all. But here’s what evidence-based plans actually look like:- Benzodiazepines: 5-10% reduction every 1-2 weeks. For someone on 10mg of diazepam daily, that’s about 0.5-1mg every two weeks. Tapers can last 4-26 weeks, depending on how long you’ve been on it.
- Opioids: 10% reduction every 5-7 days until you hit 30% of your original dose, then slower drops. The VA/DoD recommends faster tapers for people without addiction - but only if they’re stable and symptom-free.
- Antidepressants: This is the trickiest. Fluoxetine (Prozac) can sometimes be stopped in 1-2 weeks because it lingers in your system. But paroxetine (Paxil) needs 4-8 weeks. Some people use liquid forms or compounded capsules to make tiny reductions.
What to Watch For - And When to Call Your Provider
Withdrawal symptoms usually start within 1-3 days of a reduction. They’re not the same as relapse. Relapse means your original condition is coming back. Withdrawal is your body adjusting. Common signs:- Brain zaps (sudden electric-shock feelings in the head)
- Insomnia or vivid dreams
- Nausea, dizziness, or flu-like symptoms
- Increased anxiety or irritability
- Difficulty concentrating
How to Stay on Track
Tapering is a marathon, not a sprint. Here’s how to keep going:- Track your symptoms. Use a free app like Moodfit or just a notebook. Note your dose, sleep, mood, and symptoms daily.
- Set a check-in schedule. Weekly for the first month, then biweekly. Your provider should initiate these - if they don’t, ask.
- Have a backup plan. Know who to call after hours. Many clinics now offer 24/7 nurse lines for tapering patients.
- Don’t isolate yourself. Tell a trusted friend or family member what you’re doing. Withdrawal can make you feel like you’re going crazy. Having someone say, “That’s normal,” helps more than you think.
What If Your Provider Refuses?
Some providers still believe tapering is unnecessary or fear liability. If yours says, “You’re fine on this dose,” or “I don’t do tapers,” you have options.- Ask for a referral to a pain specialist, psychiatrist, or addiction medicine provider.
- Request a second opinion. You have the right to one.
- Bring printed guidelines: ASAM’s 2022 benzodiazepine tapering guide or the CDC’s 2022 opioid recommendations. Show them you’ve done your homework.
What Comes After the Last Pill
Stopping doesn’t mean you’re done. Many people need support after tapering ends - especially if the medication was masking anxiety, depression, or chronic pain. Ask your provider:- What signs should I watch for in the next 3-6 months?
- Should I schedule a follow-up in 1 month? 3 months?
- Are there non-drug strategies we can build on - therapy, exercise, sleep hygiene?
Final Thought: You’re Not Broken for Wanting to Stop
Wanting to stop a medication doesn’t mean you failed. It means you’re taking control. The goal isn’t to be on fewer pills - it’s to live better. And that’s something you deserve to talk about, without shame, without pressure, and with a provider who listens.Can I stop my medication cold turkey if I feel fine?
Even if you feel fine, stopping certain medications abruptly can trigger withdrawal symptoms that aren’t always obvious at first. For antidepressants like paroxetine or benzodiazepines like clonazepam, symptoms like brain zaps, dizziness, or anxiety can appear days later. The body adapts to the drug over time - and removing it too fast forces your nervous system into shock. Slow tapering prevents this. Feeling fine now doesn’t mean you’re safe to stop suddenly.
How long does a medication taper usually take?
It varies by drug and individual. For benzodiazepines, tapers often last 4 to 26 weeks. Opioid tapers can be 2-8 weeks, depending on dose and stability. Antidepressants range from 1-2 weeks for fluoxetine to 4-8 weeks for paroxetine. The key isn’t speed - it’s matching the pace to your body’s response. If you’re having symptoms, slow down. If you feel steady, you might speed up slightly. Your provider should adjust based on your feedback, not a fixed calendar.
What if my symptoms get worse during tapering?
Worsening symptoms don’t always mean you need to go back to your old dose. They often mean you’re tapering too fast. Most withdrawal symptoms peak within 3-7 days after a reduction and then fade. If they’re severe - like panic attacks, suicidal thoughts, or seizures - contact your provider immediately. You may need to pause the taper, reduce the amount you cut, or temporarily add a short-term medication to manage symptoms. Never push through severe symptoms hoping they’ll go away. That’s not bravery - it’s risky.
Can I taper on my own without a doctor?
It’s strongly discouraged. Even if you’ve researched everything, you don’t have access to your full medical history, lab results, or the ability to recognize dangerous signs like serotonin syndrome or rebound anxiety. Some medications require precise dosing tools (like liquid formulations or compounded capsules) that only a pharmacy can provide. Plus, without medical supervision, you risk missing underlying conditions that the medication was managing. Tapering is safest with a provider who knows your history and can adjust in real time.
Are there tools or apps to help me track my taper?
Yes. Apps like Moodfit, Daylio, and even a simple Google Sheets tracker can help you log your daily dose, mood, sleep, and symptoms. Some clinics now use digital tools like ASAM’s 2024 AI-assisted tapering toolkit, which generates personalized schedules based on your medication and health data. Writing things down helps you spot patterns - like “I always feel dizzy on Wednesday” - and gives your provider clear data to work with. The more detailed your log, the better your taper will go.


Written by Felix Greendale
View all posts by: Felix Greendale