For someone with type 1 diabetes, managing blood sugar isn’t just a daily task-it’s a full-time job. Multiple daily injections have been the standard for decades, but more people are turning to insulin pump therapy as a smarter, more flexible option. If you’re considering this switch, you’re not alone. In the U.S., nearly 4 out of 10 people with type 1 diabetes now use a pump. And it’s not just about convenience-it’s about better control, fewer lows, and more freedom.
What Is Insulin Pump Therapy?
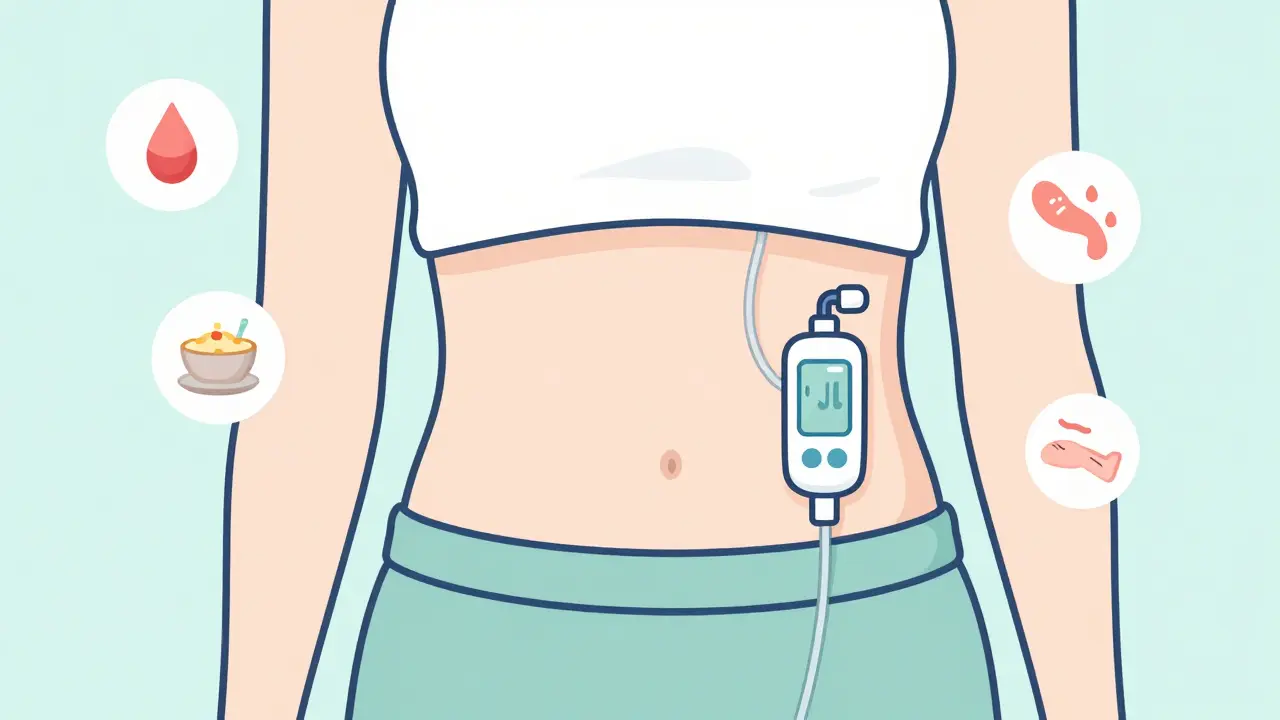
Insulin pump therapy, also called continuous subcutaneous insulin infusion (CSII), is a small wearable device that delivers rapid-acting insulin through a tiny tube or patch stuck to your skin. Unlike injections, where you give yourself shots several times a day, the pump gives you insulin 24/7 in tiny, precise amounts. You still need to bolus (give extra insulin) for meals, but the background insulin-called basal-is programmed and automatic.
Modern pumps are tiny-about the size of a small phone-and weigh less than a bar of soap. Some, like the Omnipod 5, are completely tubeless and stick directly to your body. Others, like the Medtronic MiniMed 780G or Tandem t:slim X2, use a thin tube to connect the pump to your infusion site. Most now work with continuous glucose monitors (CGMs) to automatically adjust insulin based on your real-time blood sugar levels. This is called hybrid closed-loop or automated insulin delivery (AID).
Top 5 Pros of Insulin Pump Therapy
- Better HbA1c levels - Studies show people using pumps have, on average, 0.37% lower HbA1c than those on injections. That might sound small, but it’s the difference between a high risk of complications and a much safer long-term outlook.
- Fewer nighttime lows - Pump users report 32% fewer episodes of low blood sugar while sleeping. The pump can cut insulin delivery automatically when your CGM predicts a drop, which is a game-changer for parents and people with hypoglycemia unawareness.
- More flexibility - Want to eat dinner at 9 p.m.? Skip a meal? Go for a midnight snack? Pumps let you adjust insulin on the fly. No more rigid meal schedules or carrying syringes everywhere.
- Less injection trauma - You only change your infusion set every 2-3 days. That’s 10-15 needle sticks a month instead of 30-40. For kids, teens, and needle-phobic adults, this alone makes a huge difference.
- Improved quality of life - In a survey of over 22,000 pump users, 82% said their overall quality of life improved. Many cite less mental load, fewer panic checks at night, and more confidence in social situations.
Top 5 Cons and Risks
- Technical failures happen - About 15% of users experience an insulin delivery issue at least once a month. A kinked tube, air bubble, or disconnected patch can stop insulin flow. If you don’t catch it fast, your blood sugar can spike dangerously within hours, leading to diabetic ketoacidosis (DKA).
- Higher cost and insurance hurdles - The pump itself costs $5,000-$7,000. Annual supplies (infusion sets, reservoirs, CGM sensors) run $3,000-$5,000. While 90% of U.S. patients get insurance coverage, denials still happen. Some people pay $100-$500 per year in copays; others pay thousands out of pocket.
- Learning curve is steep - You need to understand carb counting, insulin-to-carb ratios, correction factors, and how to troubleshoot alarms. Most people take 2-3 weeks to feel comfortable. One in three users make bolus calculation errors early on.
- Skin irritation and site problems - About 45% of users report redness, itching, or bumps at the infusion site. Some people can’t find a spot that doesn’t get irritated after a few days. This can lead to skipped changes and poor insulin absorption.
- Alarm fatigue and tech overload - Pumps beep, vibrate, and flash warnings constantly. For some, it’s overwhelming. One in three users say they’ve ignored alarms because they were tired of hearing them. That’s risky.

Who Is a Good Candidate?
Insulin pumps aren’t for everyone. But they’re especially helpful for:
- People with high glucose variability-blood sugar swinging wildly between highs and lows
- Those with frequent or severe hypoglycemia, especially at night
- People with hypoglycemia unawareness (no warning signs before lows)
- Anyone struggling to hit HbA1c targets despite trying multiple daily injections
- Active individuals who want freedom during exercise, swimming, or travel
- Parents of young children with type 1 diabetes-pumps make overnight management much easier
On the flip side, pumps may not be right if you:
- Have trouble with fine motor skills or can’t read small screens
- Struggle with anxiety around technology or fear of malfunctions
- Have eating disorders or difficulty with structured carb counting
- Are unwilling to check blood sugar 4-6 times a day or use a CGM
The American Diabetes Association and the Association of Diabetes Care & Education Specialists both say pump therapy should be offered to anyone with type 1 diabetes who can use it safely. But it’s not a magic fix-it’s a tool that works best when you’re ready to engage with it.
How to Get Started: Your Step-by-Step Guide
Switching to a pump isn’t a quick decision. It takes planning, education, and patience. Here’s how most people do it:
- Talk to your diabetes care team - Start with your endocrinologist or certified diabetes care and education specialist (CDCES). They’ll assess your readiness and help you decide if a pump is right for you.
- Get insurance approval - Your provider will submit paperwork to your insurance company. Be ready to show proof of HbA1c above 7.5%, recurrent lows, or other clinical reasons. If denied, appeal-it’s common.
- Choose your pump - The three main brands are Medtronic, Tandem, and Insulet. Medtronic offers the most advanced automation but uses tubing. Tandem’s Control-IQ tech is highly rated. Insulet’s Omnipod 5 is tubeless and waterproof. Try demo units if possible.
- Attend training - Most programs require 3-5 sessions over 2-4 weeks. You’ll learn how to insert the infusion set, program basal rates, calculate boluses, respond to alarms, and troubleshoot problems.
- Start with a trial - Some clinics let you use a pump with saline first to get used to wearing it. This helps you adjust to the feel and routine before insulin is involved.
- Switch over - Your provider will help you convert your daily insulin dose to pump settings. You’ll start with conservative basal rates and adjust over the next few weeks.
- Track and tweak - Keep detailed logs of your blood sugar, carbs, insulin, and activity. Review with your team weekly for the first month. Adjustments are normal.

Real Talk: What Users Say
Reddit’s r/insulinpumps community has over 15,000 members. One user, u/PumpLife2023, wrote: “The auto-basal adjustment has reduced my overnight lows from 3-4 per week to maybe once a month. I haven’t woken up panicked in months.”
But it’s not all perfect. On TuDiabetes.org, someone shared: “My Medtronic pump failed during a family vacation. I didn’t notice for 5 hours. By then, I was in DKA. Now I always carry backup pens.”
That’s the key: you must always have a backup plan. Keep fast-acting insulin and syringes or pens with you at all times. Even the best pump can fail.
What’s New in 2026?
Insulin pump tech is moving fast. In 2023, the FDA approved the Tandem t:slim X2 for kids as young as 2. The Medtronic MiniMed 880G (expected late 2024) will extend hypoglycemia safety to 150 minutes. And the Beta Bionics iLet Bionic Pancreas-currently in final trials-could be the first true “set it and forget it” system, calculating insulin needs without carb input.
By 2027, over two-thirds of new type 1 diagnoses in children will start on automated systems. That’s up from just 32% in 2022. The goal? Make technology work harder so people with diabetes can live easier.
Final Thoughts: Is It Worth It?
Insulin pump therapy isn’t easier. It’s different. It demands more attention, more learning, and more responsibility. But for many, the payoff is worth it: fewer scary lows, more freedom, and better numbers over time.
If you’re tired of juggling shots, dreading nighttime lows, or feeling trapped by your schedule-talk to your care team. Don’t assume you’re not a candidate. Don’t assume it’s too expensive. Don’t assume you’re not tech-savvy enough. The tools are better than ever. And the support is out there.
The biggest mistake? Waiting too long. The second biggest? Thinking the pump will fix everything on its own. It won’t. But with the right mindset, training, and backup plan-it can change your life.
Can children use insulin pumps?
Yes, and many do. Modern pumps like the Omnipod 5 and Medtronic MiniMed 780G are FDA-approved for children as young as 2 years old. In fact, pump use is higher among children (45%) than adults (34%) in the U.S. Parents often choose pumps because they reduce nighttime lows, simplify dosing, and eliminate the need for multiple daily injections in young kids.
Do I still need to check my blood sugar if I use a pump?
Absolutely. Even with automated insulin delivery, you need to monitor your blood sugar regularly. Most experts recommend at least 4-6 checks per day, or consistent use of a CGM. Pumps rely on accurate glucose data to make decisions. If your CGM is off or you skip calibrations, the pump can’t help you properly.
What happens if my pump breaks or stops working?
You must have a backup plan. Always carry fast-acting insulin in syringes or pens, along with alcohol wipes and a spare infusion set. If your pump fails, switch to injections immediately. Don’t wait. Insulin delivery can stop within minutes due to a kinked tube or dislodged patch. Without insulin, your blood sugar can rise fast, leading to DKA in as little as 4-6 hours.
Are insulin pumps waterproof?
Some are, some aren’t. The Omnipod 5 is fully waterproof up to 3 meters for 30 minutes, so you can swim, shower, or sweat without removing it. Tube-based pumps like the Medtronic MiniMed 780G are water-resistant but not waterproof-you need to remove them before swimming or showering. Always check the manufacturer’s specs before getting wet.
How long do insulin pumps last?
Most pumps are designed to last 4-7 years, depending on the model and usage. Insurance typically covers a new pump every 4-5 years. The device itself doesn’t wear out quickly, but technology improves fast. Many users upgrade sooner to get better automation, smaller size, or improved CGM integration.
Can I switch from a pump back to injections?
Yes, many people do. About 12% of pump users stop using them within two years due to skin issues, technical frustration, or lifestyle mismatch. Switching back to injections is straightforward-you just resume your old insulin regimen. Your care team can help you convert your pump settings back to daily doses. There’s no shame in choosing what works best for you.

Written by Felix Greendale
View all posts by: Felix Greendale