When someone says they're just feeling down, it's easy to brush it off. But major depressive disorder isn't just sadness. It's a persistent weight that makes getting out of bed, answering texts, or eating meals feel impossible. If you've been stuck in that space for weeks - or months - and nothing seems to help, you're not alone. About 1 in 6 adults in the U.S. experience this every year, and the good news is: treatment works. Not always instantly, not always the same way for everyone, but often enough to make a real difference.
What Major Depressive Disorder Really Looks Like
Major Depressive Disorder (MDD) isn't about having a bad day. It's when low mood, lack of energy, and loss of interest in things you used to love last for at least two weeks, and it starts to mess with your work, relationships, or daily life. You might sleep too much or too little. You might feel worthless, even when there's no reason to. Some people cry constantly. Others just feel numb. And here's the thing - it doesn't always start after a breakup, job loss, or death. Sometimes, it just shows up. No warning. No reason. That’s part of why it’s so confusing and isolating.
It's not a character flaw. It's not laziness. It's a real, measurable condition that affects brain chemistry, thought patterns, and even how your body functions. The DSM-5 (the manual doctors use to diagnose mental health conditions) laid out clear criteria back in 1980, and since then, we've learned a lot more about how it works - and how to treat it.
Two Main Paths: Medication and Therapy
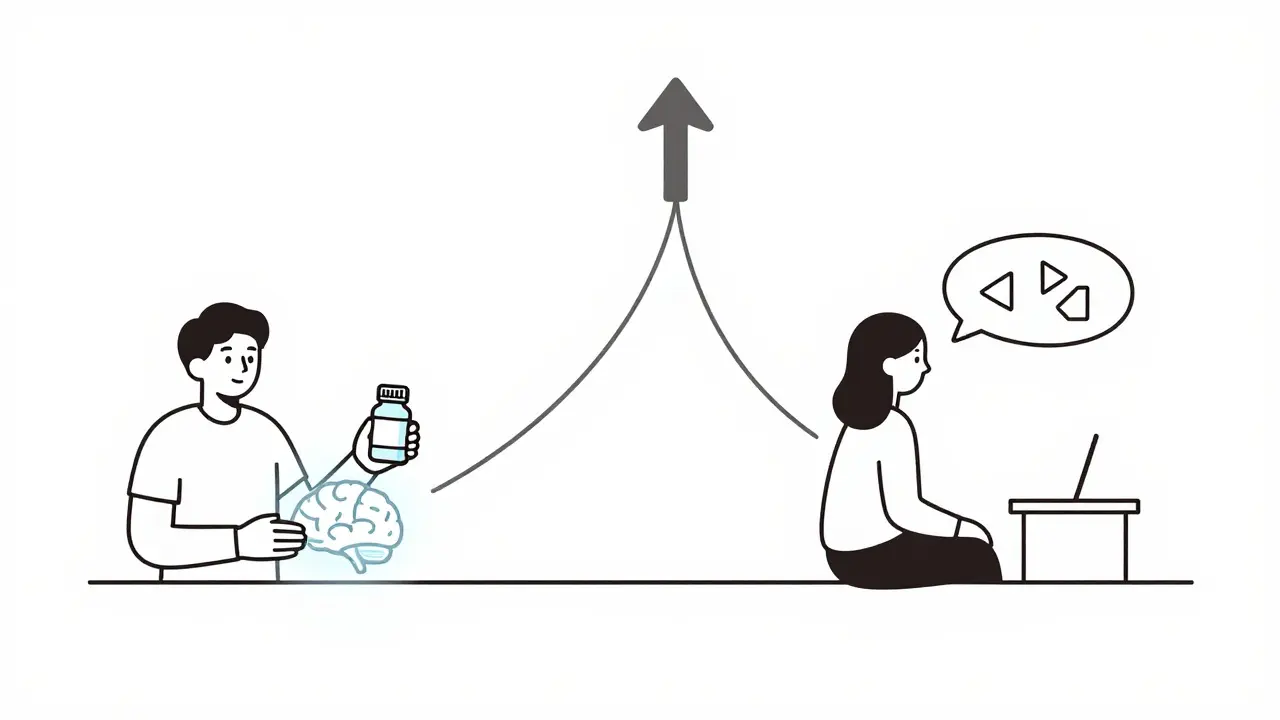
There are two primary ways to treat MDD: antidepressant medications and psychotherapy. Both have strong evidence behind them. In fact, studies show they're about equally effective on their own. But here’s where it gets important: when you combine them, you often get better results - especially if your depression is moderate to severe.
Think of it like this: medication helps rebalance your brain chemistry. Therapy helps you rebuild how you think and respond to life. One tackles the biology. The other tackles the behavior. Together, they cover more ground.
Antidepressants: What Actually Works
Not all antidepressants are the same. The most commonly prescribed are second-generation ones - meaning they're newer, safer, and have fewer side effects than older drugs. Among these, SSRIs (Selective Serotonin Reuptake Inhibitors) are usually the first try. Examples include sertraline, escitalopram, and fluoxetine. They work by increasing serotonin, a chemical linked to mood regulation.
But SSRIs aren't the only option. SNRIs (Serotonin and Norepinephrine Reuptake Inhibitors), like venlafaxine and duloxetine, also help by affecting both serotonin and norepinephrine. Some people respond better to one than the other. Then there's mirtazapine, which can help with sleep and appetite, and amitriptyline - an older drug that still works well for severe cases.
Here’s the reality: antidepressants don’t work like painkillers. You won’t feel better the next day. Most people notice small shifts after two weeks - maybe a little more energy, slightly less dread. Full effects usually take 6 to 12 weeks. And yes, some people feel worse before they feel better. Nausea, insomnia, or emotional blunting can happen early on. That’s why doctors start low and go slow.
It’s also important to know: not everyone needs medication. For mild depression, therapy alone often works fine. For severe depression (like a PHQ-9 score of 16 or higher), combining meds with therapy is strongly recommended.
Psychotherapy: More Than Just Talking
Psychotherapy isn’t about lying on a couch and talking about your mom. It’s structured, goal-oriented, and backed by science. The most well-researched approach is Cognitive Behavioral Therapy, or CBT. It works by helping you spot and change thought patterns that feed depression - like “I’m a failure” or “Nothing ever goes right.” You don’t just talk about them. You test them. You write them down. You challenge them. Over time, your brain learns new ways to think.
Another effective option is Behavioral Activation. It sounds simple: get back into activities you used to enjoy. Even if you don’t feel like it. Go for a walk. Call a friend. Cook a meal. The idea is that action comes before motivation. Doing something - even small - can slowly rebuild your sense of control.
Then there’s Interpersonal Therapy (IPT). This one focuses on relationships. If your depression is tied to grief, conflict, loneliness, or life transitions, IPT helps you work through those dynamics. It’s especially useful for people who feel stuck in unhealthy patterns with partners, family, or coworkers.
And for those who can’t access in-person therapy? Computerized CBT (CCBT) is an option. Online programs like those offered through the NHS give you structured modules you can do at your own pace. They’re not a replacement for human connection, but they’re better than nothing - especially if you live far from a therapist or have mobility issues.
Combining Both: Why It Often Wins
Studies from the Cleveland Clinic and the NHS both point to the same thing: when you use antidepressants and therapy together, you’re more likely to recover fully and stay recovered. Why? Because medication can lift the heavy fog enough for you to actually do the work in therapy. And therapy gives you tools so you don’t fall back into the same patterns once the meds are done.
One person I spoke with - a teacher in Brighton - started on sertraline after months of feeling empty. After six weeks, she still felt numb. But she started CBT. Slowly, she began noticing how she blamed herself for every small mistake. Her therapist helped her reframe it. Within four months, she was sleeping better, laughing again, and even going back to painting - something she hadn’t touched in years. She stayed on medication for a year, then tapered off. She still uses CBT techniques today.
That’s the goal: not just to feel okay for a few months, but to build resilience.

What Doesn’t Work (and Why)
Some people try therapy and give up after one or two sessions because they didn’t “feel better.” That’s like quitting a gym after one workout. Therapy is a skill. It takes time. Most people need 12 to 20 sessions to see real change.
Others switch antidepressants every few weeks because they didn’t see results. But that’s not how they work. You need at least 6-8 weeks to tell if a medication is helping. And if one doesn’t work, it doesn’t mean they all won’t. There are over 20 approved antidepressants. Finding the right one can take trial and error.
Also, don’t confuse online self-help apps with real therapy. Apps can be useful for tracking mood or offering mindfulness exercises, but they’re not a substitute for a trained therapist. The human connection matters. The accountability. The tailored feedback.
Side Effects and Risks
Antidepressants can cause side effects. Nausea, weight gain, sexual dysfunction, drowsiness - these are common, especially early on. For some, they fade after a few weeks. For others, they stick around. That’s when your doctor adjusts the dose or switches you to another drug. It’s not failure. It’s fine-tuning.
Therapy has fewer physical risks, but it can stir up painful emotions. You might cry more. You might feel angry. That’s part of healing. A good therapist will help you sit with it - not push you past it.
And while ECT (electroconvulsive therapy) is sometimes mentioned as a last-resort option for treatment-resistant depression, it’s not something most people need. It’s highly effective, but it’s reserved for severe cases that haven’t responded to anything else.
Getting Started: What to Do Now
If you think you might have MDD, start with your GP. They can screen you with a simple questionnaire (like the PHQ-9) and help you decide if you need medication, therapy, or both. In the UK, you can self-refer to NHS Talking Therapies without a referral. Wait times vary - sometimes weeks, sometimes months - but they’re there.
Don’t wait for “the right time.” Depression doesn’t care if you’re busy, tired, or scared. Treatment works best when you start early.
And if you’ve tried one thing and it didn’t work? Try another. There’s no shame in that. Recovery isn’t linear. Some people find relief with meds first. Others need therapy to even feel ready for medication. And some need both.
The goal isn’t to be perfect. It’s to be better. To get back some control. To stop feeling like you’re drowning - and start learning how to swim again.
Can antidepressants make depression worse before it gets better?
Yes, some people experience increased anxiety, agitation, or emotional numbness in the first few weeks of starting an antidepressant. This is more common with SSRIs. It doesn’t mean the medication won’t work - it often means your body is adjusting. Most side effects fade within 2-4 weeks. If they’re severe or you have thoughts of self-harm, contact your doctor immediately. Never stop medication abruptly.
How long does psychotherapy take to work for depression?
Most people start noticing small improvements after 4-6 sessions. Significant change usually takes 12-20 weekly sessions. CBT and IPT are structured therapies with clear timelines. Behavioral Activation can show results faster - sometimes in just a few weeks - because it focuses on action rather than deep analysis. Consistency matters more than speed.
Is CBT the best type of therapy for depression?
CBT is the most researched and widely recommended therapy for depression, but it’s not the only effective one. Interpersonal Therapy (IPT) works just as well for people whose depression is tied to relationship issues. Behavioral Activation is simpler and often better for those who struggle with motivation. Acceptance and Commitment Therapy (ACT) helps people who feel stuck in negative thoughts. The best therapy is the one you’ll stick with - and that fits your life.
Can I just use online therapy apps instead of seeing a therapist?
Online CBT apps can be helpful as a supplement, especially if you can’t access in-person care. But they’re not a replacement. A real therapist adapts to your responses, builds trust, and helps you navigate emotional resistance. Apps can’t read your tone, catch subtle cues, or offer support during a crisis. Use them as a tool - not a solution.
What if I can’t afford therapy or medication?
In the UK, NHS Talking Therapies are free. You can self-refer online or by phone. Many community centers also offer low-cost counseling. For medication, generic SSRIs like sertraline are inexpensive. If cost is a barrier, talk to your GP - they can help you find options. Support groups, online forums, and helplines like NAMI (800-950-6264) or text "NAMI" to 62640 can also connect you to resources.
Do antidepressants change your personality?
No. They don’t make you happy or turn you into someone else. What they do is reduce the intensity of depressive symptoms - the constant sadness, fatigue, or hopelessness - so you can feel like yourself again. Some people say they feel "numb," but that’s often because the depression was so heavy that even normal emotions felt muted. As the depression lifts, your natural emotions return - including joy, anger, and frustration - which is a good sign.


Written by Felix Greendale
View all posts by: Felix Greendale