G6PD Deficiency Antibiotic Safety Checker
This tool helps you identify safer antibiotic options based on your risk factors for G6PD deficiency. It is not a substitute for medical advice, but can help you have informed discussions with your doctor.
Your Risk Profile
Antibiotic Safety Comparison
| Antibiotic | G6PD Risk Level | Key Information | Recommendation |
|---|---|---|---|
| Nitrofurantoin | High Risk |
Common UTI treatment, but can cause life-threatening hemolytic anemia in G6PD-deficient patients Especially dangerous for pregnant women and infants |
Avoid unless G6PD status is confirmed
|
| Fosfomycin | Low Risk |
Single-dose treatment, minimal risk for G6PD deficiency Effective for uncomplicated UTIs |
Preferred alternative
|
| Cephalexin | Low Risk |
First-generation cephalosporin, minimal hemolytic risk Effective for many UTIs |
Safe alternative
|
| Pivmecillinam | Low Risk |
Common in Europe/Canada, no known hemolytic risk Limited availability in US |
Safe alternative
|
| TMP-SMX | Medium Risk |
Common UTI treatment but carries some hemolytic risk Less risky than nitrofurantoin but not risk-free |
Use with caution, test for G6PD deficiency
|
| Ciprofloxacin | Low Risk |
Effective against many bacteria but has other side effects Not associated with hemolytic anemia |
Safe alternative
|
Key Recommendations
Important Safety Information
For individuals with G6PD deficiency or from high-risk ethnic backgrounds:
- Ask your doctor about G6PD testing before taking any oxidant drugs
- Nitrofurantoin should be avoided if G6PD deficiency is present or suspected
- Fosfomycin and cephalexin are generally safer alternatives
- If you experience fever, shortness of breath, yellow skin, or dark urine while on nitrofurantoin, stop the drug and seek immediate medical attention
When you get a urinary tract infection, your doctor might prescribe nitrofurantoin. It’s cheap, effective, and widely used-over 5.5 million prescriptions are filled in the U.S. every year. But here’s something most people don’t know: if you have G6PD deficiency, this common antibiotic can trigger a dangerous, even life-threatening reaction called hemolytic anemia.
What is G6PD deficiency?
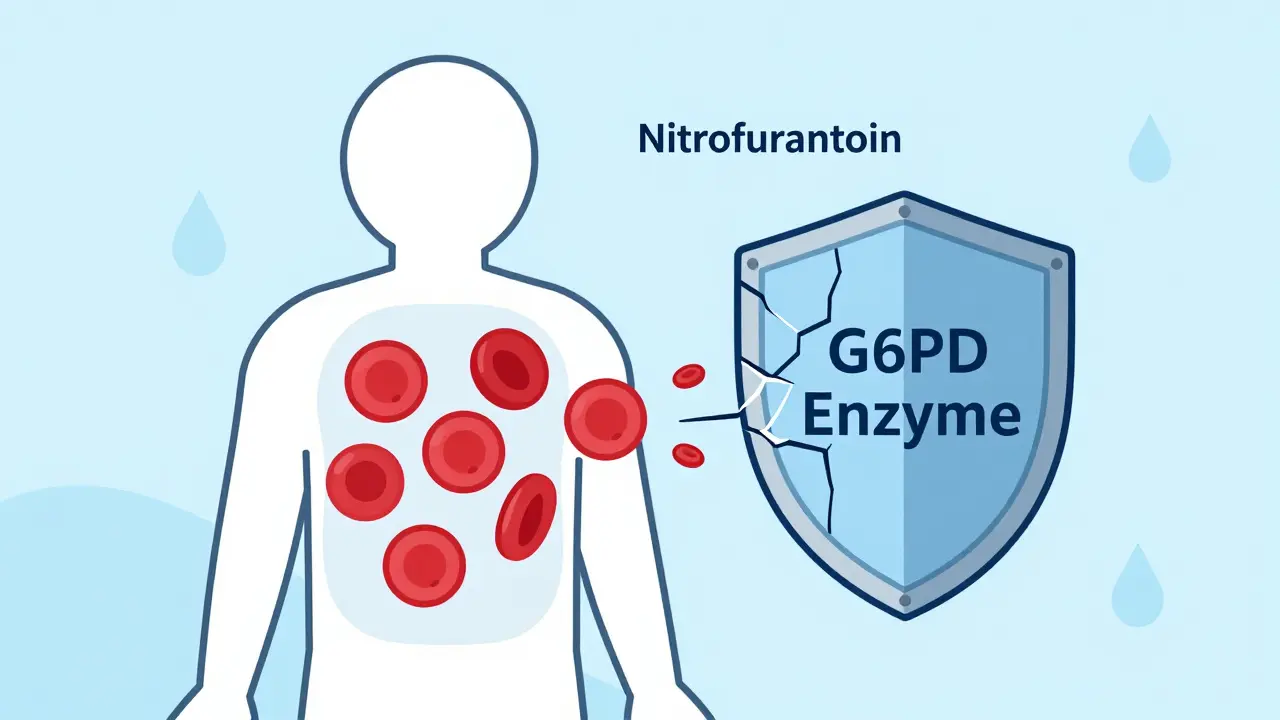
G6PD deficiency is a genetic condition where your red blood cells don’t make enough of an enzyme called glucose-6-phosphate dehydrogenase. This enzyme is like a shield-it protects your red blood cells from damage caused by certain chemicals and drugs. Without enough of it, those cells break apart too easily under stress, leading to hemolytic anemia.
It’s not rare. Around 400 million people worldwide have it, according to the World Health Organization. It’s most common in people of African, Mediterranean, Middle Eastern, and Southeast Asian descent. In Black populations, up to 14% may be affected. But here’s the problem: most people don’t know they have it until something like nitrofurantoin triggers a crisis.
How nitrofurantoin causes hemolytic anemia
Nitrofurantoin works by creating toxic compounds in your urine to kill bacteria. That’s great for treating UTIs. But in people with G6PD deficiency, those same compounds spill over into the bloodstream and attack red blood cells. The cells can’t handle the oxidative stress. Hemoglobin inside them clumps up, the cells burst, and your body can’t replace them fast enough.
The signs come fast-often within 24 to 72 hours of starting the drug. You might feel feverish, dizzy, or short of breath. Your skin or eyes could turn yellow. Dark urine, rapid heartbeat, and low blood pressure are red flags. In severe cases, kidney damage or shock can follow.
Studies show at least 42 confirmed cases of nitrofurantoin-induced hemolytic anemia in G6PD-deficient patients. Ten of those ended in death. One 2023 case report described a patient whose hemoglobin dropped from 13 g/dL to 7 g/dL in just three days-enough to require hospitalization. The good news? Stopping the drug usually leads to full recovery within 48 hours, as long as you get fluids and supportive care.
Who’s at risk?
It’s not just adults. Infants exposed to nitrofurantoin through breast milk or during pregnancy have also developed hemolytic anemia. Pregnant women with G6PD deficiency are especially vulnerable. Yet, many doctors still prescribe nitrofurantoin without checking G6PD status.
A 2022 survey of 350 primary care doctors found only 32% routinely test for G6PD deficiency before prescribing it. That’s despite clear guidelines from the American Society of Hematology and the Clinical Pharmacogenetics Implementation Consortium (CPIC), both of which say: avoid nitrofurantoin in G6PD-deficient patients.
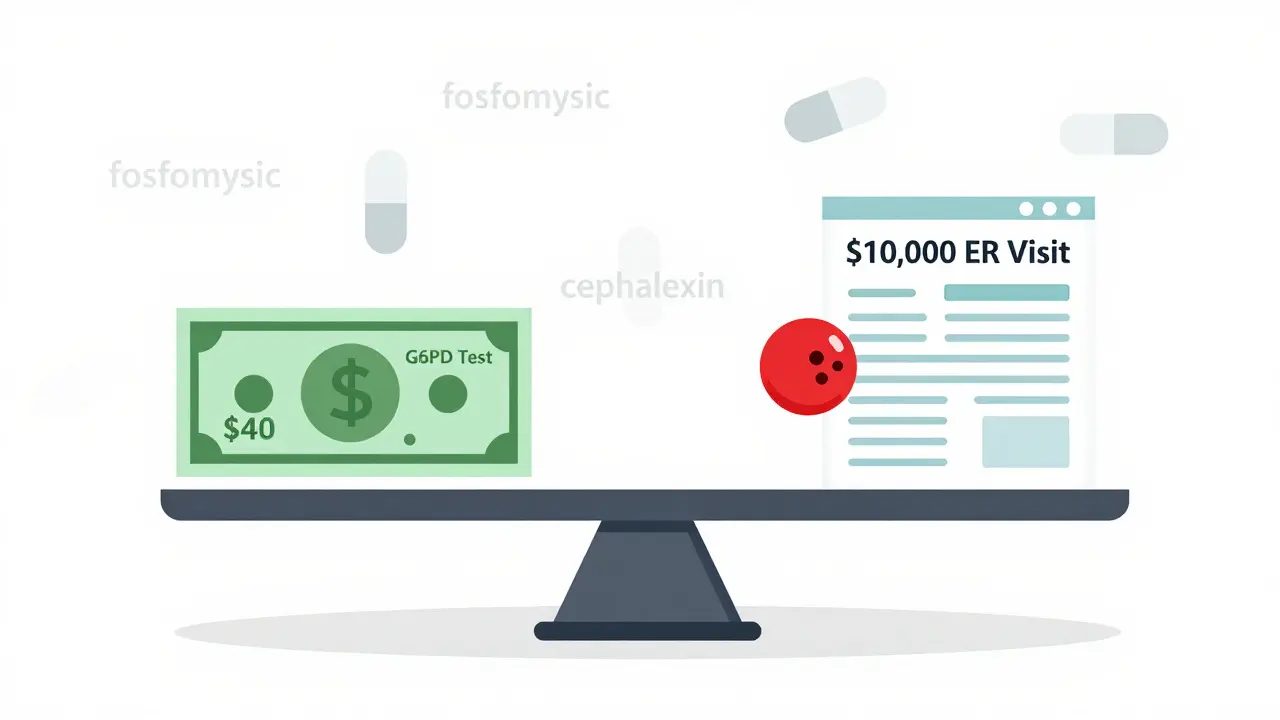
The FDA label warns about this risk-but doesn’t require testing. That’s a gap. And it’s costing lives. Hospitalization for drug-induced hemolytic anemia averages $8,500 to $12,000. A G6PD test? Around $40. The math is simple.

Alternatives to nitrofurantoin
If you have G6PD deficiency-or if you’re from a high-risk background and haven’t been tested-there are safer options.
- Fosfomycin: A single-dose antibiotic approved for uncomplicated UTIs. No known link to hemolysis.
- Cephalexin: A first-generation cephalosporin. Low risk for G6PD-related hemolysis.
- Pivmecillinam: Used in Europe and Canada, not widely available in the U.S., but effective and safe.
Trimethoprim-sulfamethoxazole (TMP-SMX) is another common choice, but it also carries some hemolytic risk-though less than nitrofurantoin. Fluoroquinolones like ciprofloxacin are effective too, but they come with their own side effects, including tendon damage and nerve issues. So, it’s not about finding the ‘best’ drug-it’s about finding the safest for you.
Why isn’t testing standard?
Some doctors argue that since G6PD deficiency is underdiagnosed, testing everyone would be too expensive. But that ignores the cost of ignoring it. In high-prevalence populations, skipping the test is like playing Russian roulette with a loaded gun.
Health systems are starting to catch on. Electronic health records now sometimes flag patients of African or Mediterranean descent when nitrofurantoin is prescribed. Some clinics in the U.S. and Europe have started routine screening for women of childbearing age before prescribing any oxidant drug.
Point-of-care G6PD tests are now available-results in 10 minutes, using a drop of blood. They’re not perfect, but they’re good enough to rule out severe deficiency. The NIH is currently running a trial to see if universal screening before nitrofurantoin use saves money and lives. Early results look promising.
What should you do?
If you’ve ever had unexplained anemia, jaundice after taking a medication, or a family history of blood disorders, ask for a G6PD test. If you’re from a high-risk ethnic group and you’re being prescribed nitrofurantoin, say no until you know your status.
Don’t assume your doctor knows. Many don’t. Don’t assume it’s not a big deal. It is. One dose can send you to the ER.
If you’ve taken nitrofurantoin and feel unwell-especially if you’re dizzy, yellow, or have dark urine-stop the drug and get help immediately. Recovery is fast if caught early. Delayed treatment can mean organ damage or worse.
Bottom line
Nitrofurantoin is a good antibiotic-for people who can safely take it. But for millions with G6PD deficiency, it’s a hidden danger. The science is clear. The tools exist. The guidelines are in place. What’s missing is consistent action.
Before you fill that prescription, ask: Have I been tested for G6PD deficiency? If the answer is no, push for a test. Your red blood cells will thank you.

Written by Felix Greendale
View all posts by: Felix Greendale