More than 5 million cases of nonmelanoma skin cancer are diagnosed in the U.S. every year. That’s more than breast, prostate, lung, and colon cancers combined. And most of them? Basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). These aren’t rare or obscure - they’re everyday realities for millions. But here’s what most people don’t realize: even though they’re both called skin cancer, they behave in completely different ways. One grows slowly and rarely spreads. The other? It can move fast, invade deeper, and sometimes turn deadly if ignored.
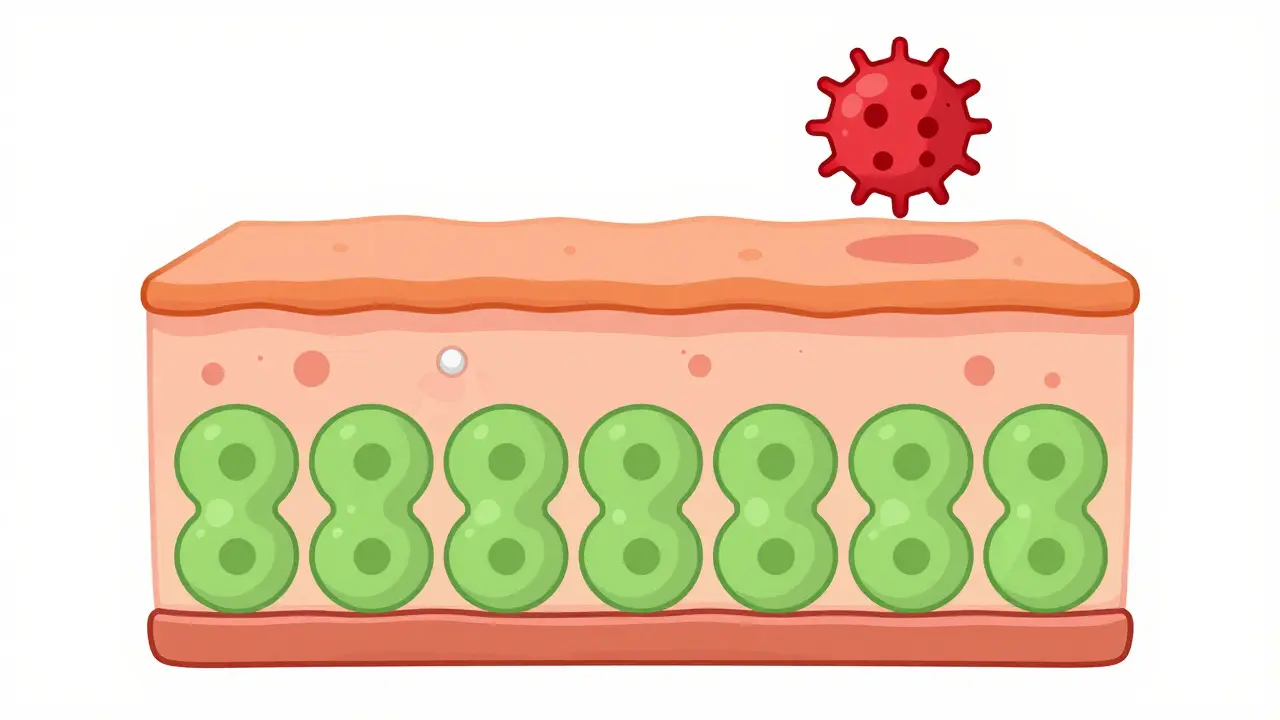
Where They Start: The Skin’s Layers
Your skin isn’t just one layer. It’s made of several, like stacked plates. The bottom layer, called the stratum basale, holds basal cells. These are the factory workers of your skin - constantly dividing to make new cells. As those new cells rise to the surface, they flatten out and become squamous cells. Think of it like a conveyor belt: basal cells at the bottom, squamous cells at the top, where they eventually flake off. Basal cell carcinoma starts in those bottom-layer basal cells. Squamous cell carcinoma starts higher up, in the squamous cells. That tiny difference in location changes everything - how they look, how they grow, and how dangerous they can become.What They Look Like: Spotting the Difference
If you’ve ever noticed a spot on your skin that won’t go away, you’re not alone. But not all spots are the same. Basal cell carcinoma often shows up as a shiny, pearly bump - especially on the face, nose, or ears. It might look like a little mole, but it doesn’t go away. Sometimes it’s an open sore that bleeds, oozes, or crusts over, then heals... only to come back again. Other times, it looks like a flat, scar-like patch that’s slightly waxy or pale. About 70% of BCCs are the pearly bump type. The rest? They’re sneaky. Squamous cell carcinoma looks different. It’s often a firm, red bump - like a wart or a rough patch that feels scaly. It might crust or bleed easily. Some SCCs look like a persistent, growing patch of dry skin that won’t respond to lotion. Around 45% of SCCs are dome-shaped bumps. Another 20% are flat, scaly red patches. These can be mistaken for eczema or psoriasis - which is why people delay seeing a doctor. Here’s the catch: both can look harmless. But if something on your skin changes shape, color, or texture over weeks - not months - get it checked. Don’t wait for it to hurt. Most of the time, it won’t.How Fast They Grow: Speed Matters
Basal cell carcinoma creeps. It grows about half a centimeter to one centimeter per year. You might notice it slowly getting bigger over months or even years. That’s why many people ignore it - “it’s been there a while,” they think. But left untreated, BCC can burrow deep into the skin, destroying cartilage, nerves, or even bone on the nose or ear. It doesn’t spread to other organs - but it can wreck your face. Squamous cell carcinoma moves faster. On average, it grows 1.5 to 2 centimeters per year. Some aggressive types can double in size in just 4 to 6 weeks. That’s not slow. That’s urgent. And while BCC stays local, SCC can spread - especially if it’s on the lips, ears, or genitals. That’s where the real danger lies.
How Dangerous They Are: The Real Risk
Let’s be clear: both are treatable. When caught early, over 95% of cases are cured. But “treatable” doesn’t mean “harmless.” Basal cell carcinoma metastasizes in fewer than 0.1% of cases. That’s one in a thousand. It’s so rare, doctors rarely worry about it spreading. But it can cause serious damage locally. About 70% of untreated BCCs invade deeper tissue after two years. That means surgery becomes more complex. Reconstruction might be needed. Scarring is common. Squamous cell carcinoma? It metastasizes in 2% to 5% of cases. That’s 20 to 50 times more likely than BCC. And when it spreads? Survival drops from 95% to 25-45%. That’s not a small difference - that’s life or death. SCC is the second leading cause of skin cancer deaths after melanoma. It doesn’t get the same attention, but it’s more dangerous. High-risk SCCs - those larger than 2 cm, deeper than 2 mm, or on the lips/ears - need aggressive treatment. Wider surgical margins. More follow-ups. Sometimes radiation or immunotherapy. The National Comprehensive Cancer Network (NCCN) says these cases need extra care. Not because they’re rare - but because they’re serious.Who Gets Them: Risk Factors
Fair skin? Sunburns? Age over 50? You’re at higher risk. About 85% of both cancers occur in people over 50. The average age at diagnosis? 67 for BCC, 69 for SCC. But there’s a gender split. Men make up 65% of SCC cases. Why? More outdoor work. More cumulative sun exposure over decades. BCC is more evenly split - 55% male, 45% female. If you’ve had an organ transplant, your risk skyrockets. Transplant patients are 250 times more likely to get SCC than the average person. For BCC? Only 10 times higher. That’s because SCC is more tied to long-term UV damage - and immunosuppressant drugs make it harder for the body to fight off cancerous cells. Geography matters too. In Australia, where sun exposure is intense, SCC makes up 30% of skin cancers. In northern Europe, it’s closer to 15%. That’s because SCC loves cumulative sun exposure - not just one bad burn. BCC? It’s more linked to intense, occasional sunburns.Treatment: What Works
Both cancers respond well to surgery. Mohs surgery - a precise technique where layers are removed and checked under a microscope - cures 99% of BCCs and 97% of SCCs. But SCC often needs wider cuts because it grows deeper. That means more tissue removed. More reconstruction. For superficial BCC, topical creams like imiquimod or 5-fluorouracil can work. They clear 60-70% of cases. For SCC? Only 40-50%. That’s why doctors rarely rely on creams for SCC. It’s too risky. If SCC has spread, things get serious. Immunotherapy drugs like cemiplimab (Libtayo) are now FDA-approved. They help the immune system attack the cancer. In advanced cases, they shrink tumors in nearly half of patients. That’s a game-changer. BCC? There’s a pill - vismodegib - that targets the hedgehog pathway, a key driver of BCC growth. It’s not used for SCC. That’s because the biology is different. One drug doesn’t fix both.

Written by Felix Greendale
View all posts by: Felix Greendale