Immunosuppressant Drug Interaction Checker
Check Your Medication Interactions
This tool checks for dangerous interactions between immunosuppressant drugs and other medications. Important: Always consult your transplant team before making any medication changes.
Interaction Results
After an organ transplant, survival isn’t just about the surgery. It’s about the daily reality of taking pills that keep your body from attacking its new organ-pills that come with a long list of side effects and dangerous interactions you can’t afford to ignore. For most transplant recipients, this isn’t temporary. It’s lifelong. And while these drugs save lives, they also reshape them in ways few people talk about.
Why You Can’t Stop Taking These Drugs
Your immune system is designed to fight off anything foreign. A transplanted kidney, liver, or heart? To your body, it’s an invader. Without drugs to suppress that response, rejection happens fast-sometimes within days. That’s why nearly all transplant patients take immunosuppressants for the rest of their lives. The only exceptions? Identical twin donors. Everything else requires medication. The standard combo? Three drugs: a calcineurin inhibitor (usually tacrolimus), an antimetabolite (like mycophenolate), and a steroid (prednisone). This triple therapy became the norm because it works. In the 1980s, kidney graft survival was around 50% after one year. Today, thanks to these drugs, it’s over 90%. But that success comes at a cost.How the Drugs Work (And Why They Cause Problems)
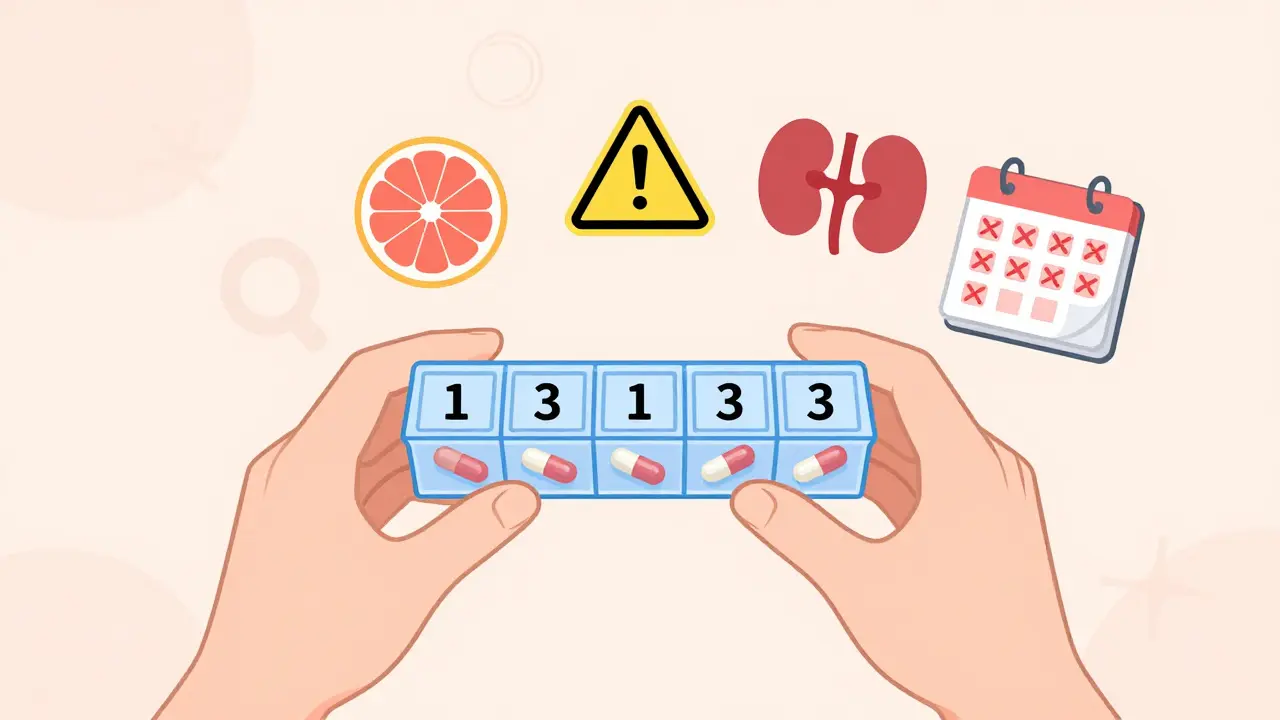
Each drug attacks rejection in a different way. Tacrolimus and cyclosporine block T-cells-the immune system’s soldiers-from activating. Mycophenolate stops those cells from multiplying. Prednisone douses inflammation across the whole body. It’s a multi-pronged attack, and it’s effective. But it’s also messy. These drugs don’t just target the bad cells. They hit everything. That’s why side effects are so common. Tacrolimus, for example, is metabolized by the same liver enzyme (CYP3A4) that processes over 50% of common medications. That means a simple antibiotic, antifungal, or even grapefruit juice can spike your drug levels to dangerous highs-or drop them so low that rejection kicks in.The Most Common Drug Interactions You Must Avoid
Some interactions are deadly. Take azole antifungals like fluconazole. Used for yeast infections, they can boost tacrolimus levels by up to 200%. One dose, and you could end up in the hospital with kidney failure or seizures. On the flip side, rifampin-used for tuberculosis-can slash tacrolimus levels by 90%. That’s a one-way ticket to organ rejection. Even over-the-counter stuff is risky. St. John’s wort, a popular herbal remedy for depression, is a strong CYP3A4 inducer. It can make your immunosuppressants useless. Same with calcium channel blockers like diltiazem, or certain HIV meds. Your transplant team needs to know every pill, supplement, or tea you take. No exceptions.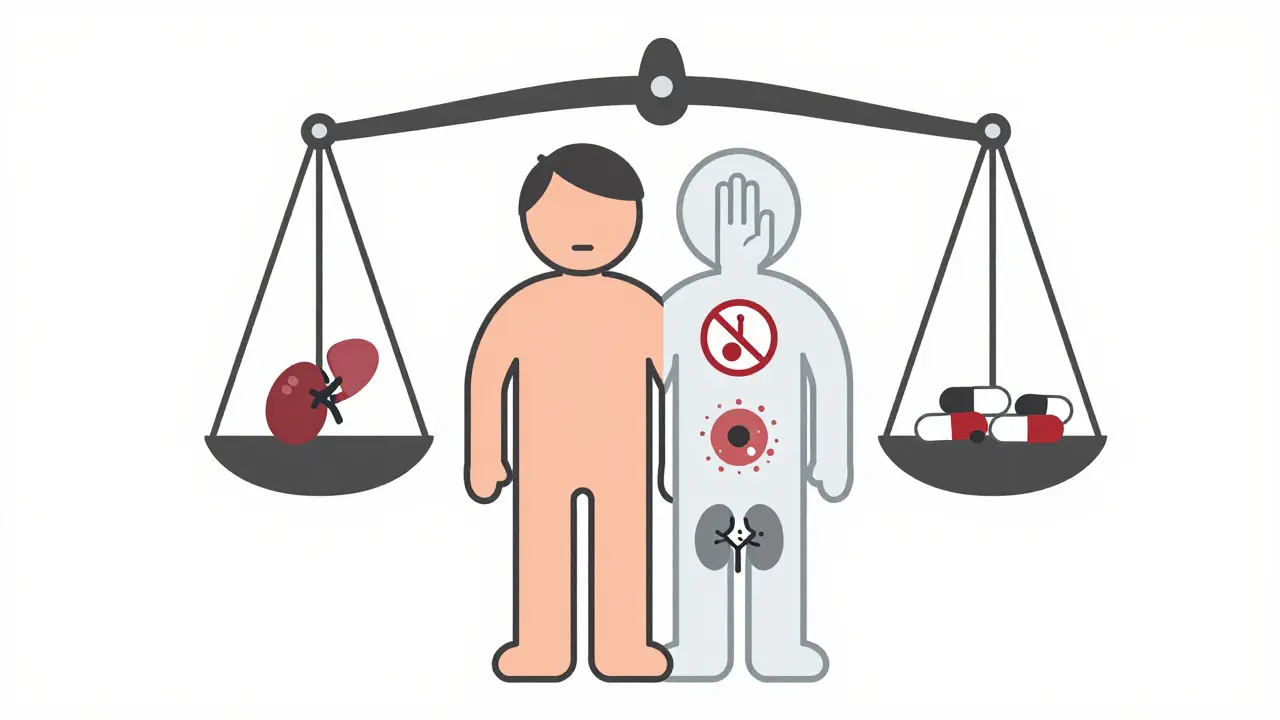
Side Effects That Change Your Life
The side effects aren’t just inconvenient-they’re life-altering. Nephrotoxicity: Up to 40% of kidney transplant patients develop chronic kidney damage from calcineurin inhibitors. By five years, 65% show scarring in biopsies. It’s ironic: the drug saving your new kidney is slowly damaging it. New-onset diabetes: Tacrolimus raises blood sugar. About 25% of recipients develop diabetes within five years. That means insulin shots, diet changes, and constant monitoring on top of everything else. Metabolic chaos: Steroids cause weight gain-15 to 20 pounds in the first six months for many. They also trigger moon face, buffalo hump, and skin thinning. One patient described looking in the mirror and not recognizing herself. Others report "steroid rage"-sudden anger, anxiety, or depression. GI nightmares: Mycophenolate causes diarrhea in over a third of users. Nausea, vomiting, abdominal pain? Common. Some patients stop taking it because they can’t tolerate it. Others switch to azathioprine, but that brings its own risk: bone marrow suppression. Low white blood cells mean more infections. Wound healing problems: mTOR inhibitors like sirolimus help protect the kidneys but delay healing. A simple cut can take weeks. Mouth ulcers? Frequent. Skin cancers? 23% of liver transplant patients get non-melanoma skin cancer. That’s 10 times higher than the general population.What Real Patients Are Saying
On Reddit, one user wrote: "I take 11 pills a day, at different times. I’ve missed doses. I’ve had to go to the ER because my levels dropped. I’m terrified of rejection, but I hate how I feel every day. My hands shake from tacrolimus. I’m always tired. I can’t eat raw vegetables because of Listeria. I wear a mask in the grocery store. Is this living?" Another switched from tacrolimus to sirolimus after his kidney function dropped. "My GFR went from 38 to 52. I felt better. But now I have mouth sores and high cholesterol. I’m on statins now. Still better than dialysis, but it’s a trade-off." The National Kidney Foundation found that 41% of transplant recipients say side effects hurt their quality of life. Chronic fatigue? 72%. Sleep problems? 68%. Emotional swings? 54%. These aren’t side effects you can ignore. They’re part of your new normal.How Doctors Manage the Risks
Transplant centers don’t just hand out prescriptions. They monitor closely. For tacrolimus, blood levels are checked twice a week at first, then weekly, then monthly. Blood counts? Monthly. Cholesterol and glucose? Every three to six months. Biopsies? Routine at one and five years. Many centers now use electronic pill dispensers. One study showed adherence jumped from 72% to 89% with them. Why? Because missing a dose can trigger rejection. And rejection often leads to graft loss-and back to dialysis or waiting lists. Steroid minimization is becoming standard. Most leading centers now stop prednisone within two weeks for low-risk patients. That cuts diabetes risk by 30%, reduces weight gain, and lowers bone loss.
New Hope on the Horizon
There’s progress. Voclosporin, approved in 2023, causes less kidney damage than tacrolimus. Belatacept, a newer drug, cuts heart disease and cancer risk-but increases early rejection. It’s not perfect, but it’s a step forward. The biggest breakthrough? Tolerance. In a 2023 trial, 15% of kidney transplant patients stopped all immunosuppressants entirely after receiving regulatory T-cell therapy. Their bodies didn’t reject the organ. No drugs. No side effects. It’s still experimental, but it’s proof that lifelong medication isn’t the only future.What You Need to Do Right Now
If you’re on immunosuppressants:- Keep a written list of every medication, supplement, and herb you take. Show it to every doctor, even your dentist.
- Never start or stop anything without talking to your transplant team.
- Avoid raw meat, unpasteurized dairy, and unwashed produce. Listeria can kill you.
- Wear sunscreen daily. Skin cancer is common and aggressive.
- Report fever above 100.4°F immediately. It could be infection, not a cold.
- Live within two hours of your transplant center-especially in the first year. Emergencies don’t wait.
The Hard Truth
Transplant recipients live longer than they used to. But they still die younger than people their age who never needed a transplant. Ten-year survival? 65% for kidney recipients. For healthy peers? 85%. The drugs keep you alive, but they also wear you down. The goal isn’t just survival. It’s quality. That’s why research is pushing for tolerance, better drugs, and steroid-free regimens. But until then, the balance is razor-thin. Too little drug? Rejection. Too much? Side effects that break your body and your spirit. You’re not just a patient. You’re someone managing a complex, lifelong chemical tightrope. And you’re not alone. But you have to be your own advocate. Because no one else will know your body like you do.Can I stop taking my immunosuppressants if I feel fine?
No. Feeling fine doesn’t mean your immune system isn’t slowly attacking your transplant. Most rejection happens without symptoms until it’s too late. Stopping medication-even for a few days-can trigger irreversible damage. Lifelong immunosuppression is required for almost all transplant recipients. The only exceptions are rare cases of operational tolerance achieved through experimental therapies.
What should I do if I get sick and need antibiotics?
Always contact your transplant team before taking any new medication-even over-the-counter ones. Antibiotics like clarithromycin or antifungals like fluconazole can dangerously increase levels of tacrolimus or cyclosporine. Your team may adjust your dose or choose a safer alternative. Never self-prescribe.
Why do I need to avoid grapefruit?
Grapefruit and grapefruit juice block the enzyme CYP3A4 in your gut and liver. This is the same enzyme that breaks down tacrolimus and cyclosporine. When blocked, drug levels rise sharply, increasing the risk of kidney damage, nerve toxicity, and even seizures. Even small amounts can have a lasting effect-so avoid it completely.
How do I know if my drug levels are too high or too low?
You won’t feel it. That’s why regular blood tests are non-negotiable. High levels can cause tremors, headaches, high blood pressure, or kidney damage. Low levels may cause no symptoms at all-until rejection starts. Your transplant center will set target ranges based on your organ, time since transplant, and other factors. Stick to the schedule.
Are there alternatives to steroids?
Yes. Many transplant centers now use early steroid withdrawal, stopping prednisone within 7-14 days for low-risk patients. Alternatives include higher doses of mycophenolate or switching to mTOR inhibitors like sirolimus. These reduce weight gain, diabetes, and bone loss-but come with their own side effects, like high cholesterol or mouth sores. Your team will choose based on your health profile.
Can immunosuppressants cause cancer?
Yes. Suppressing your immune system reduces its ability to detect and destroy cancer cells. Skin cancers (especially squamous cell carcinoma) are the most common, affecting up to 23% of liver transplant recipients. Other risks include lymphoma, Kaposi sarcoma, and gastrointestinal cancers. Regular skin checks and avoiding UV exposure are critical. Some newer drugs, like belatacept, appear to lower cancer risk compared to calcineurin inhibitors.
What happens if I miss a dose?
If you miss one dose, take it as soon as you remember-if it’s within a few hours. If it’s been longer, skip it and resume your regular schedule. Never double up. Missing doses increases rejection risk. If you miss more than one, contact your transplant team immediately. They may check your drug levels and adjust your plan. Use pill organizers or apps to help stay on track.
Do these drugs affect fertility or pregnancy?
Some immunosuppressants are safe during pregnancy, while others are not. Mycophenolate is linked to birth defects and must be stopped months before conception. Tacrolimus and cyclosporine are generally considered safer but still require close monitoring. Always plan pregnancy with your transplant team. Many women have healthy babies after transplant, but it requires careful timing and medication adjustments.
Why do I need to live close to the transplant center?
In the first year after transplant, you’re at highest risk for rejection, infection, and drug toxicity. Emergencies can happen suddenly-like a spike in tacrolimus levels or sudden kidney failure. Living within two hours ensures you can reach your center quickly for blood tests, biopsies, or hospitalization. Most U.S. transplant programs require this as part of your care plan.
Is there a future without lifelong drugs?
Yes, but it’s still experimental. Research into regulatory T-cell therapy and mixed chimerism has allowed a small percentage of patients to stop all immunosuppressants without rejection. The ONE Study reported 15% of kidney recipients achieved this at two years. It’s not yet standard care, but it’s the most promising path toward true immune tolerance. Until then, medications remain essential.

Written by Felix Greendale
View all posts by: Felix Greendale