Symptom Reporting Impact Calculator
How Your Symptoms Compare to Clinical Documentation
This tool demonstrates the difference between what patients report versus what doctors typically document. Based on FDA data, patients report up to 40% more side effects than clinicians.
Your Reporting Impact
Key Findings
Based on FDA data:
- Patients report 30-40% more side effects than clinicians
- Fatigue reported 4.2x more often by patients
- Nerve pain reported 3.8x more often
Your reporting could have identified 0 potential treatment adjustments earlier
Why This Matters
PROs (Patient-Reported Outcomes) capture symptoms that often go unnoticed in clinical settings. In one study, patients flagged a dangerous drop in white blood cells two weeks earlier than their oncologist noticed. This early detection can prevent serious complications like hospitalization.
When you take a new medication, you’re not just a passive recipient of treatment-you’re a critical data source. Every time you note that your fatigue got worse, your hands tingled after chemo, or your sleep vanished for three nights straight, you’re contributing to something bigger than your own care. This isn’t just anecdotal. These reports are called Patient-Reported Outcomes (PROs), and they’re now a formal part of how drugs are monitored for safety worldwide.
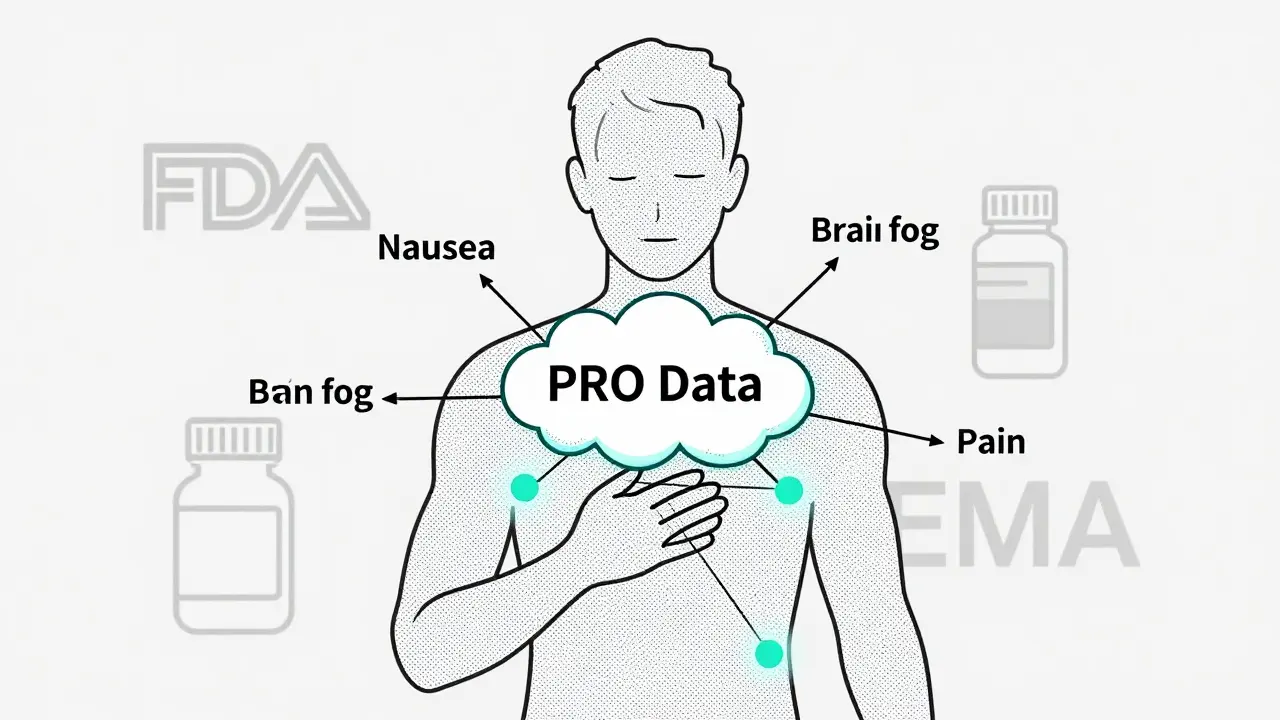
What Exactly Are Patient-Reported Outcomes?
PROs are direct reports from patients about how they feel and function, without doctors or researchers interpreting what they say. If you report that your nausea is a 7 out of 10, or that you’ve missed work because of dizziness, that’s a PRO. The U.S. Food and Drug Administration (FDA) defines them clearly: they come straight from you, no filters. This might sound simple, but it’s revolutionary. For decades, drug safety relied mostly on doctors noting side effects during clinic visits. But many symptoms-like brain fog, emotional exhaustion, or mild but persistent pain-don’t show up in blood tests or physical exams. Only you can report them.
PROs aren’t new in theory-they’ve been studied since the 1980s-but their use in drug safety really took off after 2010. That’s when the European Union and the U.S. passed laws requiring patient voices to be part of the benefit-risk evaluation for new medicines. Today, if a drug company wants approval for a cancer treatment, they must include PRO data. The FDA’s 2022 draft guidance made it official: three core areas must be tracked in cancer trials-symptoms like nausea or pain, physical function (can you walk, dress yourself?), and disease-specific issues like coughing or bleeding.
Why Your Reports Matter More Than You Think
Here’s the hard truth: doctors miss a lot. A 2019 FDA study found patients reported 30-40% more side effects than clinicians did. For fatigue? Patients reported it 4.2 times more often. For nerve pain? 3.8 times. For memory lapses or trouble concentrating? Five times more. Why? Because patients live with these symptoms every day. A doctor sees you once every few weeks. You live with the fog, the ache, the sleeplessness, the anxiety-every single hour.
PROs don’t just add numbers-they change timing. In one study, patients flagged a dangerous drop in white blood cells two weeks earlier than their oncologist noticed. That’s not a small advantage. It’s the difference between adjusting a dose safely and ending up in the hospital. One breast cancer patient on a MedHelp forum shared how using a PRO app helped her doctor reduce her chemo dose before she ended up in the ER. That’s not luck. That’s data.
And it’s not just about emergencies. PROs help catch slow-burning problems-like gradual loss of mobility, worsening depression, or chronic dry mouth-that might never make it into a clinical report unless someone asks you directly. These are the symptoms that ruin quality of life, even if they’re not immediately life-threatening. Regulatory agencies now recognize that a drug that extends life but leaves patients too exhausted to enjoy it isn’t truly successful.

How PROs Are Collected-And Why It’s Not Just Paper Forms Anymore
PROs used to mean paper questionnaires mailed to your home. Now, they’re mostly digital. Around 87% of global clinical trials use electronic PROs (ePROs) via smartphones, tablets, or web portals. These systems send you reminders, let you log symptoms in real time, and even sync with wearables. In one Pfizer trial for eczema, patients wore sensors that tracked scratching. The data matched their self-reported itch 73% of the time-proving that what you say and what your body does often line up.
But it’s not just about tech. The tools themselves have to be scientifically sound. A PRO questionnaire isn’t just a list of questions-it’s a validated instrument. That means it’s been tested on hundreds of people to make sure it’s reliable (same results over time), valid (actually measures what it claims to), and sensitive enough to detect small changes. The PRO-CTCAE, for example, has 78 symptom items rated on frequency and severity. Developing one of these takes 18-24 months and costs between $500,000 and $750,000. That’s why you’ll see the same tools used across trials: PROMIS for physical function, EORTC QLQ-C30 for cancer, ASCQ-Me for sickle cell disease.
And yes, it’s still a burden. A 2022 survey found 65% of patients felt heard-but 32% struggled with tech issues, and 27% found questions confusing. One Reddit user complained about doing three different surveys three times a week: “It became a job.” That’s a real problem. Too many questions, too often, and people quit. Smart systems now use adaptive testing-only asking follow-up questions if you report a problem-and automated reminders that boost response rates from 70% to over 90%.
The Gap Between Data and Action
Here’s the uncomfortable part: most patients don’t see what happens to their data. The same 2022 survey found 68% of participants never received feedback on how their reports influenced treatment. That’s a trust issue. If you’re spending 10 minutes every other day logging your symptoms, you deserve to know it mattered.
Some clinics are starting to change that. In oncology, providers now show patients their own PRO trends during visits-graphs of pain levels over time, sleep patterns, energy scores. This turns PROs from a research tool into a conversation starter. “Your fatigue spiked last week-what changed?” becomes a real question, not a checklist item.
But the system isn’t perfect. People without smartphones, those with low literacy, or those in rural areas still get left out. And unvalidated tools? They can mislead. Dr. Janet Woodcock, former head of the FDA’s drug center, warned that sloppy PRO instruments can distort safety signals. That’s why validation matters. Not just for regulators-but for you. Bad tools mean bad decisions. Good tools mean better care.
What’s Next? AI, Wearables, and the Future of Your Voice
The next wave is even more personal. Roche is testing AI that reads patient notes written in plain language-like “I feel like my brain is full of cotton”-and turns them into coded adverse events with 82% accuracy. That means your words, not just your checkboxes, are being analyzed. Wearables are getting smarter too. Imagine your smartwatch detecting increased heart rate and restlessness during a panic attack, then prompting you to log it. That’s not sci-fi-it’s already in trials.
Blockchain is being used by Novartis to keep your PRO data private and secure, so you control who sees it. And by 2026, the European Medicines Agency plans to require PRO data for nearly all new drug applications. This isn’t a trend. It’s the new baseline.
Drug safety is no longer just about lab results and death rates. It’s about how you live. Your fatigue. Your anxiety. Your ability to play with your kids or go to work. That’s what matters. And now, it’s part of the science.
How You Can Make Your Voice Count
If you’re in a clinical trial or taking a new medication, here’s what you can do:
- Take PRO surveys seriously-even if they feel repetitive. Your answers help others.
- Use the app or portal. Don’t wait until your next appointment. Report symptoms as they happen.
- Ask: “Will my answers be used to change my treatment?” If the answer is no, push for clarity.
- If you struggle with tech, ask for help. Many trials offer phone-based PRO systems.
- Share your experience. If you felt heard, say so. If you felt ignored, speak up. Your feedback improves the system.
You don’t need to be a scientist to make a difference. You just need to be honest. Your body knows what it’s going through. And now, the system is finally listening.


Written by Felix Greendale
View all posts by: Felix Greendale