One minute you’re walking up the stairs, and the next, you can’t catch your breath. No fever. No cough. No asthma inhaler helps. Your chest feels tight, but your lungs sound fine when the doctor listens. This isn’t anxiety. It’s not just being out of shape. It could be a pulmonary embolism - a blood clot blocking an artery in your lung. And it’s more common than most people think.
What Exactly Is a Pulmonary Embolism?
A pulmonary embolism (PE) happens when a blood clot, usually from a deep vein in your leg, breaks loose and travels to your lungs. About 70% of these clots start in the deep veins of the lower legs - a condition called deep vein thrombosis (DVT). Once the clot reaches the pulmonary arteries, it blocks blood flow. Your lungs can’t oxygenate your blood properly. Your heart has to work harder. And if the clot is large enough, it can stop your heart entirely. The scary part? You might not see it coming. Unlike a heart attack with crushing chest pain, PE often sneaks in with vague symptoms. The most common sign - sudden shortness of breath - shows up in 85% of cases. It doesn’t come on slowly. It hits hard, even if you were sitting still watching TV. People describe it like trying to breathe through a straw while running a sprint.Other Symptoms You Can’t Ignore
Shortness of breath is the big red flag, but it rarely comes alone. Here’s what else to watch for:- Chest pain - sharp, stabbing, worse when you breathe in or cough. It’s often mistaken for a heart attack. About 74% of PE patients report this.
- Cough - dry at first, but in 23% of cases, you might cough up blood.
- Leg swelling - one leg, usually the calf, feels swollen, warm, or tender. This is your body’s warning that a clot started there.
- Fast heartbeat - over 100 beats per minute without exercise or stress.
- Dizziness or fainting - happens in about 14% of cases. This is a medical emergency.
Why Diagnosis Is So Hard - And So Critical
PE is called a "great mimicker" because its symptoms overlap with so many other conditions: pneumonia, asthma, panic attacks, even muscle strain. That’s why it’s often missed. In the U.S., around 100,000 people die from PE each year - many because it wasn’t caught in time. Doctors don’t rely on one test. They use a step-by-step process. First, they assess your risk using tools like the Wells Criteria or Geneva Score. These aren’t guesswork. They’re evidence-based checklists that weigh things like recent surgery, cancer, leg swelling, and heart rate. A trained clinician using these tools can correctly identify low-risk patients 89% of the time. If your risk is low, the next step is a D-dimer blood test. D-dimer measures a protein fragment that’s released when clots break down. A negative result (below 500 ng/mL) means PE is extremely unlikely - 97% accurate in low-risk people. But here’s the catch: if you’re over 50, the test becomes less reliable. That’s why doctors now use age-adjusted thresholds: for every year over 50, you add 10 ng/mL to the normal limit. This cuts down on unnecessary scans by more than a third.The Gold Standard: CTPA Scans
If your risk is moderate or high - or if your D-dimer is positive - the next step is almost always a CTPA: a computed tomography pulmonary angiogram. This is a specialized CT scan that uses contrast dye to show the blood vessels in your lungs. It finds clots in 95% of cases and misses very few. The scan takes less than 10 minutes. You lie on a table, an IV is placed in your arm, and you’re asked to hold your breath while the machine takes images. Radiation exposure is low - about the same as a cross-country flight. But it’s not for everyone. If you’re allergic to iodine or have kidney problems, doctors turn to a V/Q scan - a nuclear medicine test that checks airflow and blood flow in the lungs. It’s less common, but still highly accurate when used properly. Some hospitals now use ultrasound to check your legs for DVT. If they find a clot in your thigh or calf, and you have symptoms like shortness of breath, they can treat you for PE without waiting for a scan. This saves time - and lives.
What Happens in the ER? Real-Life Scenarios
In the emergency room, things move fast when PE is suspected. If you’re unstable - passing out, low blood pressure, turning blue - doctors skip the D-dimer and go straight to an echocardiogram. This ultrasound of your heart can show if your right ventricle is strained from the clot. If it is, you’re having a massive PE. You need clot-busting drugs or even emergency surgery. One hospital in California cut their time-to-scan from over two hours to under 45 minutes by creating a dedicated PE pathway. Mortality dropped from 8.2% to 3.1%. That’s not just statistics - that’s people going home. On the flip side, patients like SarahK_42 on the American Lung Association’s forum shared how they were told it was anxiety for weeks. She was climbing stairs and gasping - but doctors didn’t order a scan until she collapsed. By then, the clot had grown.Who’s at Risk? It’s Not Just the Obvious Cases
Most people think PE only happens to older, overweight people who sit too long. But the truth is more complex.- Cancer patients have nearly five times the risk. Their blood is more prone to clotting.
- Recent surgery - especially hip, knee, or abdominal - raises risk for up to three months.
- Pregnancy and birth control - estrogen increases clotting risk.
- Genetic conditions - like Factor V Leiden - make some people clot more easily.
- Long flights or car rides - sitting for more than four hours without moving.
What Comes After Diagnosis?
Once PE is confirmed, treatment starts immediately. Blood thinners - like heparin or warfarin - are the first line. They don’t dissolve the clot. They stop it from getting bigger while your body breaks it down naturally over weeks or months. For massive clots that cause shock, doctors may use clot-busting drugs (thrombolytics) or a catheter to pull the clot out. These are high-risk procedures - but they save lives. Most people take blood thinners for at least three months. If you had a first PE with a clear trigger - like surgery - you might stop after that. But if the clot came out of nowhere, or you have cancer or a genetic clotting disorder, you might need to stay on them for life.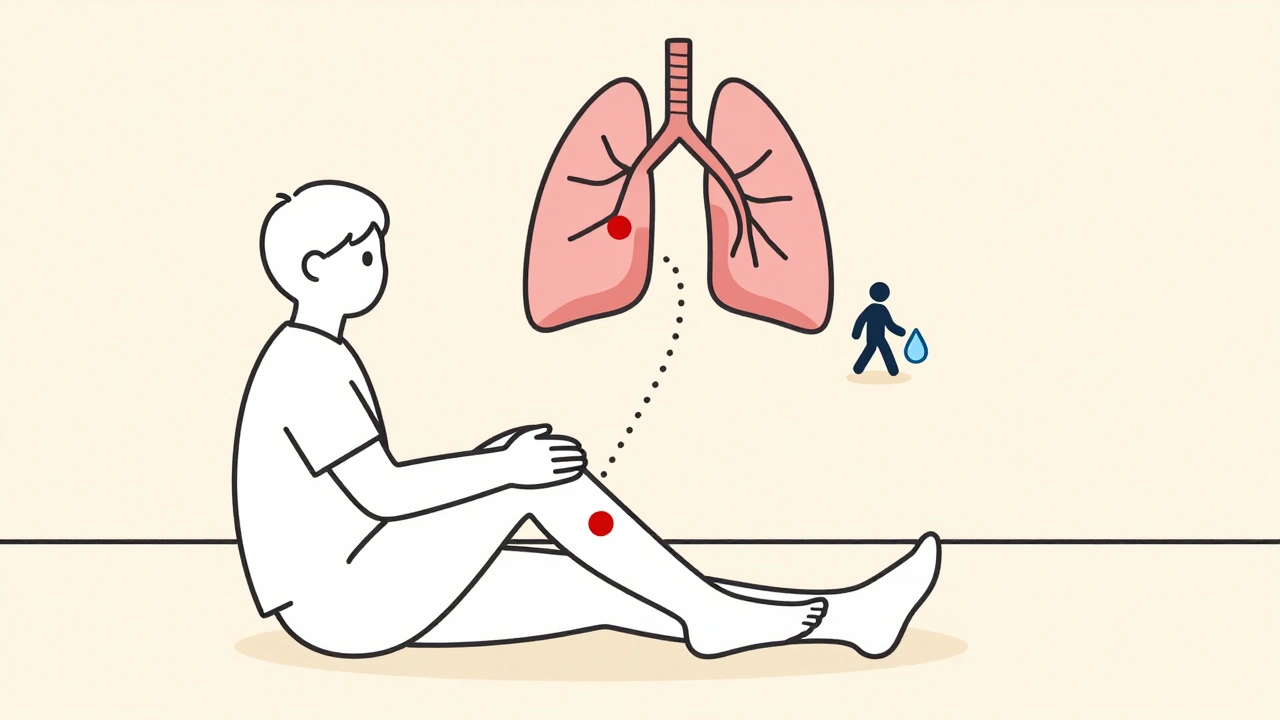
Can You Prevent It?
Yes - and it’s simpler than you think.- Move your legs during long trips. Stand up, walk, flex your ankles.
- Stay hydrated. Dehydration thickens your blood.
- If you’re hospitalized, ask about compression stockings or anticoagulant shots.
- If you’ve had one PE before, your risk of another is 33% within 10 years. Talk to your doctor about long-term prevention.
What’s New in PE Diagnosis?
Technology is catching up. Artificial intelligence is now helping radiologists read CTPA scans. One AI tool, PE-Flow, detected clots with 93.7% accuracy - matching or beating human experts. Another breakthrough? Blood tests that combine D-dimer with other markers like soluble thrombomodulin. Early trials show these panels can rule out PE with 98.7% accuracy in intermediate-risk patients. That means fewer scans, less radiation, faster answers. Hospitals are also forming Pulmonary Embolism Response Teams (PERT) - multidisciplinary groups of specialists who act fast when a major clot is found. Since 2015, these teams have cut treatment delays and reduced deaths by over 4%.Final Thought: Trust Your Body
If you suddenly can’t breathe - and it doesn’t make sense - don’t dismiss it. Don’t wait for a second opinion. Don’t let someone tell you it’s stress. Go to the ER. Ask: "Could this be a pulmonary embolism?" The tools to find it exist. The treatments work. But they only help if you speak up - and if your doctor listens.Can you have a pulmonary embolism without knowing it?
Yes, especially if the clot is small. Some people have minor PE symptoms - like mild shortness of breath or a dry cough - and assume it’s allergies or a cold. These clots can still grow or lead to another clot later. Even "silent" PEs can damage lung tissue over time. If you’ve had unexplained breathlessness, it’s worth checking.
Is a pulmonary embolism the same as a heart attack?
No. A heart attack happens when a clot blocks blood flow to the heart muscle. A pulmonary embolism blocks blood flow to the lungs. Both are medical emergencies, but they affect different organs. Chest pain from PE is usually sharp and gets worse with breathing. Heart attack pain is often crushing, pressure-like, and may spread to the arm or jaw.
How long does it take to recover from a pulmonary embolism?
Recovery varies. Most people feel better in a few weeks, but full recovery can take months. Fatigue and breathlessness linger as your lungs heal. Blood thinners are usually taken for at least three months. Some people need them longer. Physical activity helps - but you should start slowly and under medical guidance.
Can you get a pulmonary embolism from sitting too long?
Yes. Sitting still for more than four hours - on a plane, car, or even at a desk - increases risk. Blood pools in the legs, which can trigger a clot. This is why doctors recommend moving your legs, wearing compression socks, and staying hydrated during long trips. It’s not just for older people - even young, healthy travelers are at risk.
Are blood thinners dangerous?
All medications have risks. Blood thinners can cause bleeding - from nosebleeds to serious internal bleeding. But the risk of dying from an untreated PE is far higher. Doctors weigh your risk of clotting versus bleeding before prescribing. Newer blood thinners are safer than older ones like warfarin, with fewer dietary restrictions and no need for frequent blood tests.
Can you exercise after a pulmonary embolism?
Yes - and you should. Light walking helps improve circulation and prevents new clots. Most people can resume normal activity within a few weeks. Avoid intense workouts until your doctor says it’s safe. If you feel dizzy, short of breath, or have chest pain during exercise, stop and call your doctor. Exercise is part of recovery, not a threat to it.


Written by Felix Greendale
View all posts by: Felix Greendale