When your doctor orders pulmonary function tests, it’s usually because you’re short of breath, have a chronic cough, or they’re trying to figure out why your lungs aren’t working like they should. Two of the most important tests in this group are spirometry and DLCO. They’re not the same thing, and they don’t tell you the same thing. But when you put them together, they give you a clear picture of what’s really going on in your lungs.
What Spirometry Measures - and What It Misses
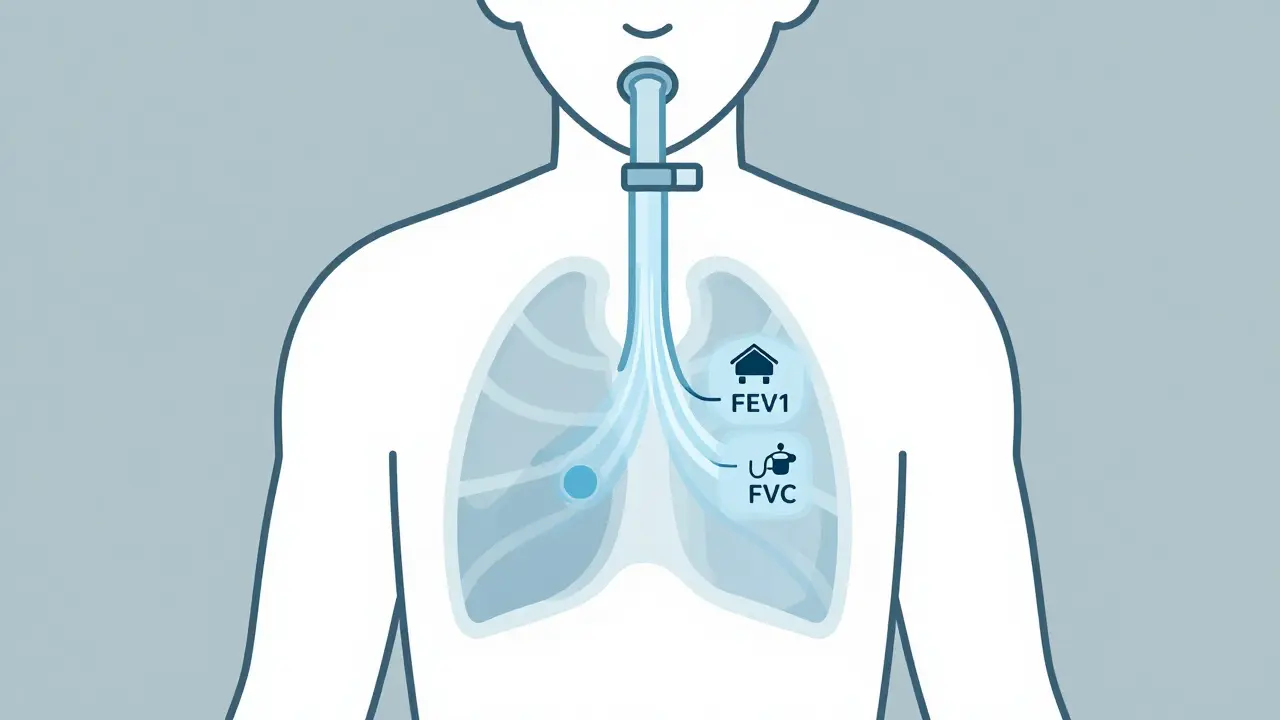
Spirometry is the most common lung test you’ll ever take. You breathe into a tube as hard and fast as you can after taking the deepest breath possible. It measures two key numbers: forced vital capacity (FVC) - the total amount of air you can blow out - and forced expiratory volume in one second (FEV1) - how much air you can blow out in the first second. The magic number is the FEV1/FVC ratio. If this ratio is below 0.7, you have airflow obstruction. That means something is blocking or narrowing your airways - like in asthma or COPD. If the ratio is normal but your FVC is low, that suggests restriction - your lungs aren’t expanding fully. But here’s the trap: sometimes, your lungs are stuck full of air (called air trapping), and that can make your FVC look low even if your lungs aren’t actually stiff. That’s called pseudorestriction. Spirometry alone can’t tell the difference.What DLCO Tells You - The Missing Piece
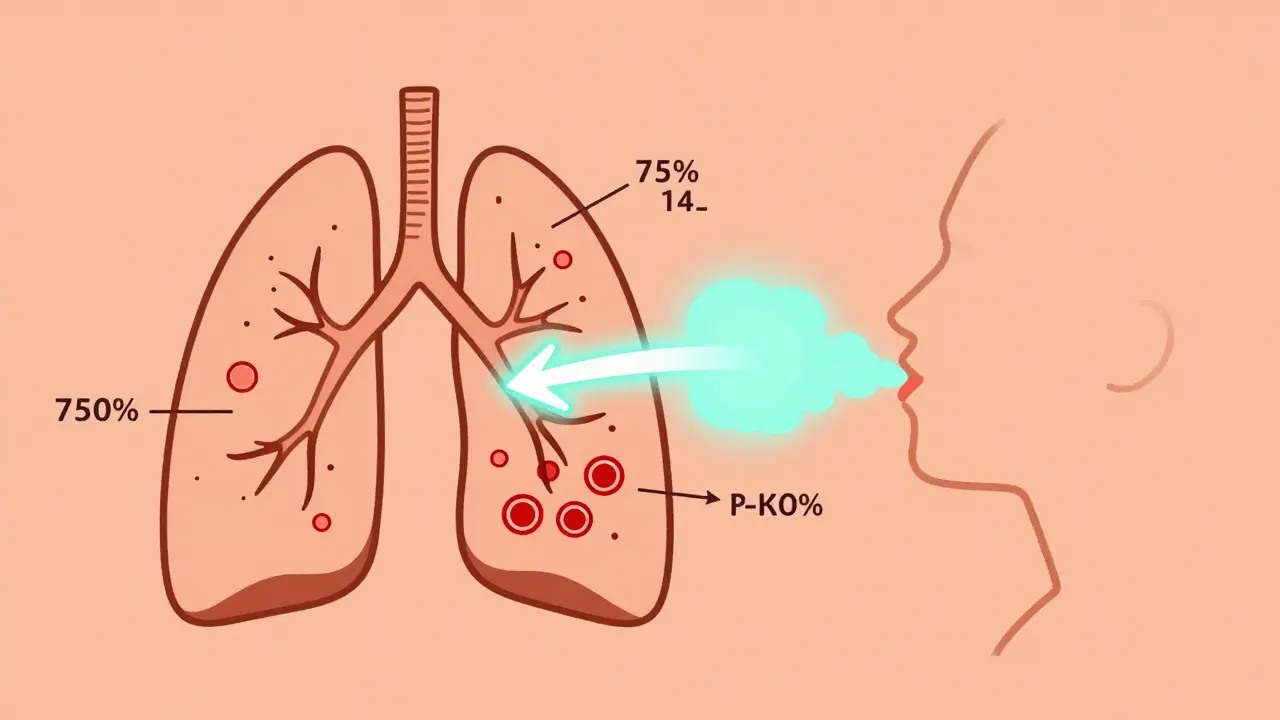
DLCO stands for diffusing capacity of the lung for carbon monoxide. Sounds complicated? It’s not. It’s really just measuring how well oxygen moves from your lungs into your blood. You inhale a tiny bit of carbon monoxide (harmless at this level), hold your breath for 10 seconds, then exhale. The machine measures how much CO was absorbed - and that tells doctors how efficiently your lungs transfer gas. Normal DLCO is between 75% and 140% of what’s predicted for your age, height, and sex. Below 75% means your lungs aren’t transferring oxygen well. Above 140% means they’re doing better than expected - which can happen in conditions like asthma or anemia. The real power of DLCO is what it reveals when spirometry doesn’t. For example:- If your FVC is low but your DLCO is normal, your lungs are probably restricted because of something outside the lung tissue - like obesity, scoliosis, or a weak diaphragm.
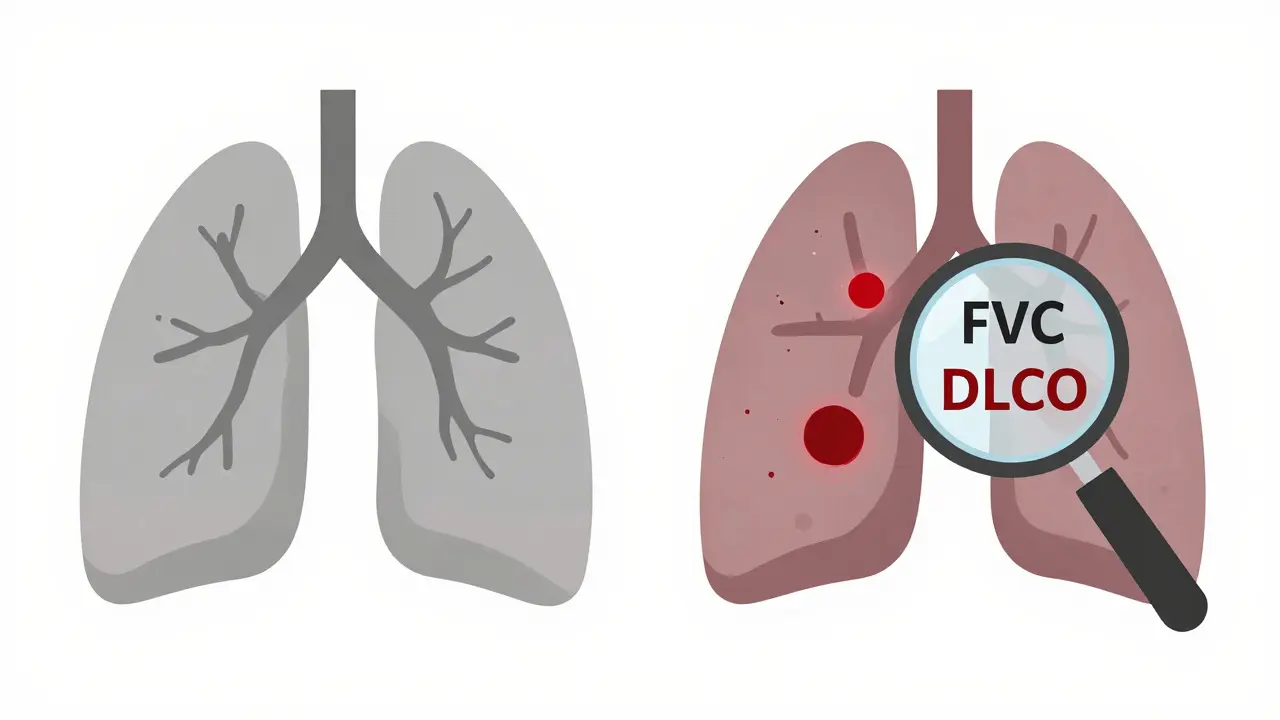
- If your FVC is low and your DLCO is also low, you likely have damage inside the lung - like pulmonary fibrosis or emphysema.
- If your spirometry is completely normal but your DLCO is low? That’s a red flag for early interstitial lung disease, pulmonary hypertension, or even small blood clots in the lungs.
How Doctors Use the Two Tests Together
Think of spirometry as the first question: “Are your airways blocked?” Then DLCO is the follow-up: “Can your lungs actually deliver oxygen?” Here’s how it works in practice:- Normal spirometry + normal DLCO - Your lungs are healthy.
- Low FEV1/FVC ratio - Obstruction. Could be asthma, COPD, or cystic fibrosis. DLCO helps here too: if DLCO is low, it suggests emphysema or advanced disease. If DLCO is normal or high, it points more toward asthma.
- Low FVC with normal FEV1/FVC - Restriction. Now check DLCO. If DLCO is low, it’s likely a lung disease like fibrosis. If DLCO is normal, it’s probably a chest wall or muscle problem.
- Normal spirometry + low DLCO - This is where things get interesting. You might have early lung scarring, small vessel disease, or pulmonary hypertension. In fact, DLCO drops before spirometry changes in early interstitial lung disease - sometimes by 12 to 18 months.
Why DLCO Is Often Overlooked - And Why You Should Care
Many doctors don’t order DLCO routinely. It’s more expensive. It’s harder to perform. Some patients can’t hold their breath for 10 seconds. But skipping it is like trying to diagnose a heart problem with only an EKG and no blood test. Here’s what happens when DLCO is ignored:- A patient with early pulmonary fibrosis gets told “your lungs are fine” because spirometry looks normal - but their DLCO is at 65%. They miss the window for early treatment.
- A person with unexplained shortness of breath and normal spirometry is labeled “anxious.” But their DLCO is 58% - they have undiagnosed pulmonary hypertension.
- A patient with asthma has a normal DLCO, so their doctor assumes they’re well-controlled. But if DLCO was high (135%), it might mean they’re having frequent flare-ups with inflammation.
- Patients with connective tissue diseases (like scleroderma or lupus) - lung damage often shows up first as a drop in DLCO.
- People being evaluated for lung surgery - low DLCO means higher risk of complications.
- Those with unexplained breathlessness - especially if they’re young, non-smokers, or have no history of asthma.
The Hidden Factors That Can Skew Your Results
DLCO isn’t perfect. It’s sensitive to things you might not think matter:- Hemoglobin - Every 1 g/dL drop in hemoglobin lowers DLCO by about 1%. If you’re anemic, your DLCO will look falsely low. That’s why labs must measure your hemoglobin before testing.
- Carbon monoxide exposure - Even smoking a cigarette 12 hours before the test can raise your carboxyhemoglobin and lower your DLCO by 5-10%.
- Alveolar volume - If you don’t hold your breath long enough or leak air, the test gets messed up. That’s why trained technicians are essential.
- Altitude - At high elevations, DLCO naturally increases. Reference values must be adjusted.
What’s Next? New Tools and Future Directions
AI is starting to help. In 2023, a Mayo Clinic study showed algorithms could predict pulmonary hypertension from DLCO patterns with 88% accuracy - just by looking at the shape of the curve, not just the number. New guidelines from the American Thoracic Society now require hemoglobin correction as standard practice. And in clinical trials for new fibrosis drugs, DLCO is now a key outcome - not just FVC. The bottom line? DLCO isn’t a backup test. It’s a frontline tool. If you have lung symptoms and your spirometry doesn’t explain them, ask for DLCO. It might be the difference between being told “nothing’s wrong” and getting the right diagnosis before it’s too late.Common Questions About Pulmonary Function Tests
Can I do spirometry and DLCO on the same day?
Yes, most clinics do both tests in one visit. Spirometry comes first because it’s simpler and doesn’t require special preparation. DLCO follows after, usually with a 10- to 15-minute break so you can recover from the deep breaths. If you’re very tired or short of breath, the technician might delay DLCO to ensure accurate results.
Is DLCO painful or dangerous?
No. The gas you inhale contains a tiny, safe amount of carbon monoxide - far less than you’d get from smoking one cigarette. You won’t feel anything during the test. Some people feel lightheaded from holding their breath, but that passes quickly. There’s no radiation, needles, or risk involved.
Why is DLCO low in emphysema but normal in asthma?
Emphysema destroys the tiny air sacs (alveoli) where gas exchange happens. Fewer sacs = less surface area to transfer oxygen = low DLCO. In asthma, the airways swell, but the alveoli stay intact. In fact, during a flare-up, more blood flows to the lungs, which can make DLCO go up. That’s why a high DLCO can actually suggest active asthma.
Can I get a false low DLCO if I’m anemic?
Yes. Hemoglobin carries oxygen in your blood. If you’re low on it, your lungs may transfer gas just fine, but there’s less hemoglobin to pick it up. That makes DLCO look artificially low. That’s why labs must check your hemoglobin before the test - and why doctors correct the DLCO value based on your actual level. Without this correction, you might be misdiagnosed.
What if my DLCO is high?
A high DLCO (over 140%) can mean several things: asthma during a flare-up, extra red blood cells (polycythemia), a heart shunt that sends too much blood to the lungs, or even bleeding into the lung tissue. It’s not always a problem - some healthy people naturally have higher values. But when it’s paired with symptoms like shortness of breath or fatigue, it’s a clue that needs further investigation.

Written by Felix Greendale
View all posts by: Felix Greendale