When a spinal cord injury happens, it doesn’t just break bones-it breaks the connection between your brain and the rest of your body. The damage can mean losing movement, feeling, or even control over bladder and bowel function. What follows isn’t just medical treatment-it’s a long, hard rebuild of independence. And that rebuild starts the moment you’re stable enough to begin.
What Gets Lost After a Spinal Cord Injury?
The effects of a spinal cord injury depend entirely on where the damage occurs and how severe it is. A fracture at the C3 level? You might lose the ability to breathe without a ventilator. A T12 injury? You could lose leg movement but still have full arm function. It’s not a one-size-fits-all situation.Motor function loss means muscles below the injury go quiet. Some people experience spasticity-muscles that suddenly tighten, jerk, or cramp uncontrollably. Others go completely limp. Sensory loss can mean no feeling of heat, pain, or pressure. That’s dangerous. You might not notice a pressure sore forming on your tailbone until it’s deep and infected.
Autonomic functions get hit hard too. Blood pressure can drop dangerously low when sitting up. Bladder and bowel control often vanish. Managing them takes time-45 to 90 minutes a day, every day. And temperature regulation? Forget sweating or shivering normally. You’re at higher risk for heatstroke or hypothermia without realizing it.
Statistics show 17,810 new cases happen every year in the U.S. alone. Most come from car crashes, falls, or violence. But here’s the thing: survival rates have climbed because emergency care got better. Now the real challenge is what comes after.
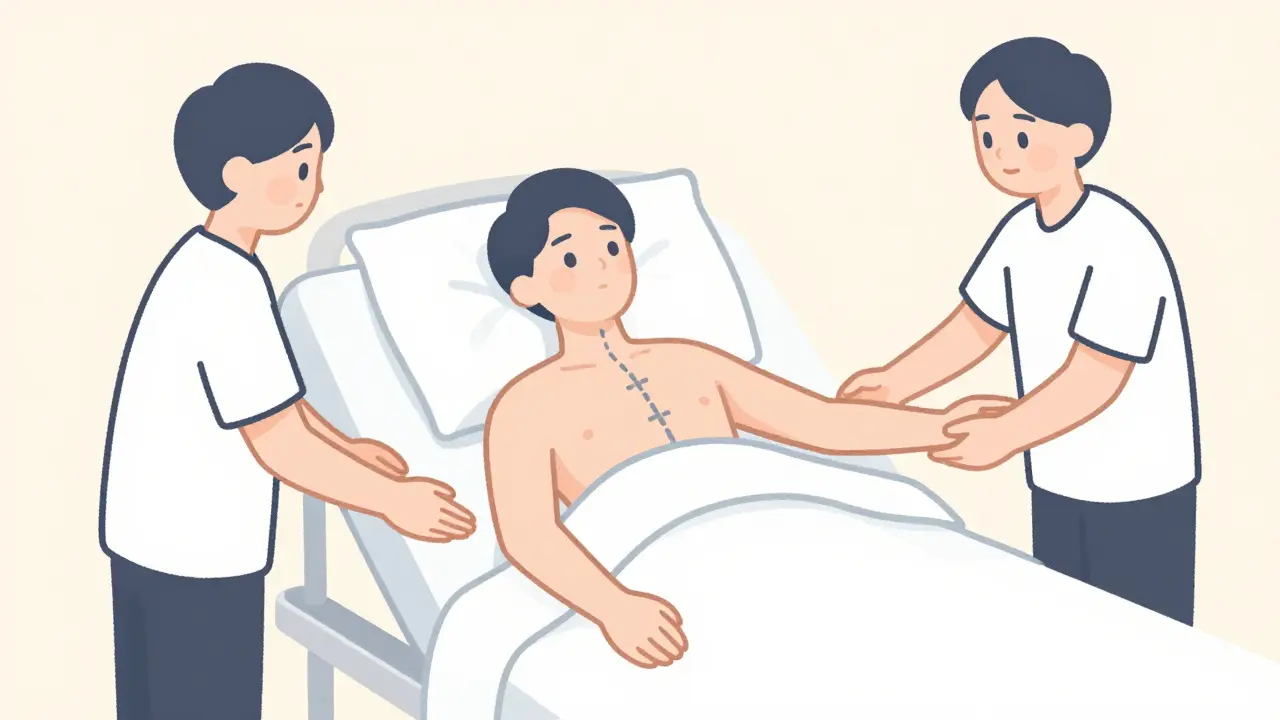
Rehabilitation: It Starts in Hours, Not Weeks
Rehab doesn’t wait. It begins within 24 to 72 hours after you’re medically stable. That’s not a suggestion-it’s standard. Delaying means muscles stiffen, joints lock, and lungs fill with fluid. Preventing those complications is half the battle.Every day in rehab, you get at least three hours of therapy, five days a week. Not just one therapist. A whole team: physical therapists, occupational therapists, nurses, psychologists, social workers. They work together to rebuild what’s broken.
Passive range-of-motion exercises are non-negotiable. If you can’t move your arms or legs, someone else does it for you-once daily if you’re flaccid, two or three times if you’re spastic. Skipping these means permanent contractures. Your elbows might freeze bent. Your hips could lock shut.
For cervical injuries (C1-C4), shoulder mobility is critical. For C5-C6, elbow and wrist positioning matters most. A small mistake in positioning during early rehab can lead to lifelong pain and disability.
One of the biggest advances? Treadmill training with body weight support. Instead of just practicing walking on the floor, you’re suspended over a treadmill with a harness. Sensors adjust your weight, and therapists guide your legs. Studies show this method improves walking speed by 23% more than regular overground training. It doesn’t just move your legs-it rewires your brain’s walking circuits.
Assistive Devices: From Wheelchairs to Exoskeletons
You don’t walk again? That doesn’t mean you’re stuck. Assistive devices turn limitations into manageable routines.Wheelchairs are the foundation. But not just any chair. A custom seating system with pressure-relieving cushions, tilt-in-space frames, and power-assist wheels can cost $2,500 to $5,000. Medicare covers 80% after your deductible-but you still pay $1,200 to $3,500 out of pocket. Many people skip upgrades because of cost.
Then there are the high-tech options. Functional Electrical Stimulation (FES) bikes use small electric pulses to make paralyzed muscles pedal. One study found FES cycling increased oxygen use by 14.3%-far more than regular arm cycling. Users report less muscle loss, better circulation, and even improved mood. But home units cost $5,000. Insurance rarely covers them.
Exoskeletons like Ekso and ReWalk let some people stand and take steps again. One user on Reddit said, “I took my first steps in three years with Ekso.” But each session lasts only 25 to 45 minutes. You need three therapists to help you into it. And the machine weighs 45 pounds. It’s not practical for daily use-yet.
Robotic arms like Armeo help those with hand paralysis relearn grip and reach. Diaphragm pacing implants, FDA-approved in 2022, let people with high cervical injuries breathe without a ventilator 74% of the time. These aren’t sci-fi anymore. They’re real. But access? That’s still uneven.
The Real Barriers: Money, Motivation, and Follow-Up
The science is there. The tools exist. But what stops people from getting better?Insurance. Medicare won’t cover every device. Private insurers often deny FES bikes, exoskeletons, or home therapy equipment. Many patients abandon rehab because they can’t afford it.
Motivation fades fast. A survey found 68% of people stop doing home exercises within six months. Why? No one checks in. No accountability. No peer support.
That’s where peer counseling changes everything. At Spaulding Rehabilitation, 82% of patients said talking to someone who’d been through it made them feel less alone. One woman told her therapist, “I didn’t think I’d ever laugh again. Then I met someone who could joke about using a catheter like it was a coffee mug.”
And caregivers? They’re often overlooked. Improper lifting causes 32% of shoulder injuries in family members and nurses. Training them isn’t optional-it’s essential. You can’t rehab your body if your caregiver’s in pain too.
The Future: AI, Implants, and Personalized Recovery
The next five years will change everything.AI-driven therapy plans are rolling out in 65% of top rehab centers by 2025. Instead of a fixed routine, your progress adjusts in real time. If your leg strength plateaus, the system changes your exercises. If your spasticity spikes, it recommends new meds or timing.
Brain-computer interfaces are in early trials. One study in Nature Medicine showed 38% improvement in hand function for people with C4 injuries-just by thinking about moving their fingers. The device reads brain signals and moves a robotic hand. It’s not perfect. But it’s working.
Implantable diaphragm pacers are already here. They’re not just for emergencies. People are living longer, more active lives because of them.
The biggest shift? From “rehab until you’re stable” to “rehab until you’re thriving.” It’s no longer about learning to live with a disability. It’s about rebuilding a life.
What Recovery Really Looks Like
Complete paraplegics? Only 1-3% regain walking ability. Incomplete injuries? Up to 59% do. That’s the difference between a full break and a partial one.But numbers don’t tell the whole story. One man with a T6 injury didn’t walk again. But he learned to use an FES bike, started cycling with a local group, and now coaches others. Another woman with a C6 injury regained enough hand function to paint again. She sells her art online.
Recovery isn’t about going back to who you were. It’s about becoming someone new-with new strengths, new tools, and new reasons to keep going.
Can you fully recover from a spinal cord injury?
Complete recovery is rare. Only 1-3% of people with complete paraplegia regain walking ability. But for those with incomplete injuries, up to 59% can regain some mobility. Most people, regardless of injury level, improve significantly in independence, bladder/bowel control, and quality of life with proper rehab. Recovery is measured in function gained, not just movement restored.
How soon should rehab start after a spinal cord injury?
Rehab begins within 24 to 72 hours after medical stabilization. Early intervention prevents muscle atrophy, joint contractures, and lung infections. Even if you’re still in the hospital, passive range-of-motion exercises, breathing support, and positioning start immediately. Delaying rehab increases long-term disability risk.
Are exoskeletons worth the cost for SCI patients?
Exoskeletons like Ekso and ReWalk offer psychological and physical benefits-standing, stepping, improved circulation-but they’re not practical for daily use. Sessions are limited to 30-45 minutes, require 2-3 therapists, and cost $100,000+ per unit. Insurance rarely covers them. For most, they’re a tool for therapy, not mobility. Their real value is in motivation and preventing secondary health issues.
What’s the most important part of SCI rehab?
Preventing secondary complications. That means daily passive stretching, pressure sore prevention, respiratory care, and bowel/bladder management. Without these, even the best mobility gains can be undone by infection, pain, or hospitalization. The goal isn’t just to move-it’s to stay healthy enough to keep moving.
Why do so many people stop doing home exercises?
Lack of structure and support. Without regular check-ins, goal-setting, or peer encouragement, exercises become chores. A 2022 survey found 68% of patients quit home programs within six months. Those with peer mentors or telehealth follow-up were three times more likely to stick with them.
Can insurance cover advanced rehab tech like FES bikes or exoskeletons?
Medicare and private insurers cover some devices, but not all. Wheelchairs and basic mobility aids are often approved. FES bikes, exoskeletons, and home systems are frequently denied or only partially covered. Out-of-pocket costs can run $5,000-$100,000. Many patients rely on grants, nonprofit programs, or fundraising to access these tools.

Written by Felix Greendale
View all posts by: Felix Greendale