TCA Blood Level Checker
Check Your TCA Blood Level Safety
Therapeutic drug monitoring for tricyclic antidepressants is essential to prevent life-threatening toxicity. Enter your blood level to see if it's within the safe therapeutic range for your specific medication.
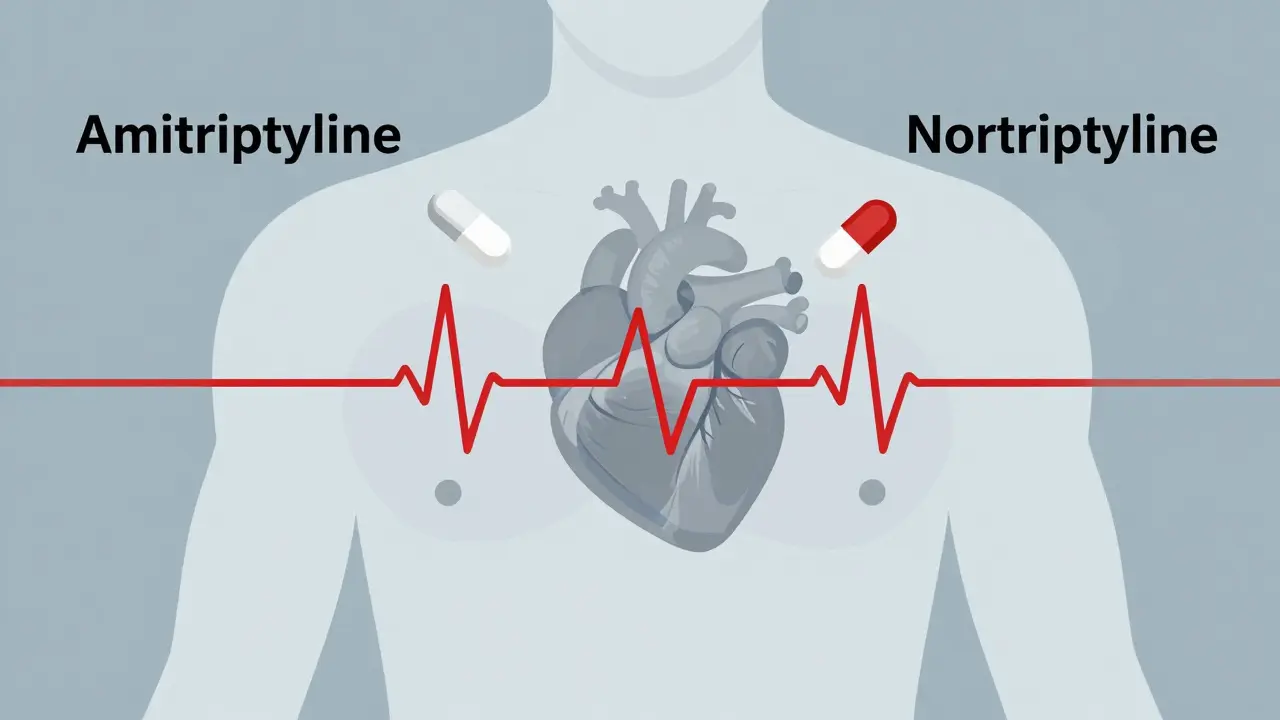
Tricyclic antidepressants (TCAs) like amitriptyline and nortriptyline aren’t used as often as they used to be. But for some people-especially those with treatment-resistant depression or chronic nerve pain-they’re still the most effective option. The problem? These drugs have a razor-thin margin between helping and harming. A single extra pill can push blood levels into the danger zone. That’s where therapeutic drug monitoring comes in. It’s not optional. It’s lifesaving.
Why TCAs Are So Dangerous
TCAs work by boosting serotonin and norepinephrine in the brain. But they don’t stop there. They also block receptors in your heart, nerves, and digestive system. That’s why side effects like dry mouth, blurred vision, and constipation are common. But when levels climb too high, things turn deadly.At blood concentrations above 500 ng/mL, TCAs can shut down your heart’s electrical system. The QRS complex on an ECG widens past 100 milliseconds. Your heart rhythm goes haywire. You can slip into seizures, coma, or sudden cardiac arrest. And here’s the scary part: you don’t need to overdose on purpose. A 75 mg dose of amitriptyline-perfectly normal for one person-can be toxic for another. That’s because metabolism varies wildly. Some people break down TCAs slowly. Others clear them too fast. Genetics, age, liver function, and other medications all play a role.
Studies show TCAs cause 15-20% of fatal prescription overdoses, even though they’re only prescribed in about 3.5% of antidepressant cases. That’s five to ten times more deadly than SSRIs like fluoxetine or sertraline. And it’s not just accidental overdoses. Elderly patients on steady doses can still build up toxic levels over weeks due to slower metabolism. One study found that 40% of TCA users are over 65. For them, even a small increase in dose can be catastrophic.
What Therapeutic Drug Monitoring Actually Measures
Therapeutic drug monitoring (TDM) isn’t just checking if you’re taking your pills. It’s measuring exactly how much of the drug is in your blood-and whether your body is turning it into active or harmful metabolites.For amitriptyline, the safe range is 80-200 ng/mL. Nortriptyline? 50-150 ng/mL. Desipramine? 100-300 ng/mL. These aren’t guesses. They’re based on decades of clinical data linking blood levels to both effectiveness and toxicity. But it’s not enough to just get a number. Timing matters. Blood must be drawn right before your next dose-called a trough level-after at least five to seven days of consistent dosing. Why? Because it takes that long for your body to reach a steady state. Draw blood too early, and the result is meaningless.
The test itself uses high-performance liquid chromatography or mass spectrometry. Labs take 24 to 48 hours to return results. That delay is a problem. But it’s still better than waiting for someone to collapse. The real value of TDM is catching problems before they become emergencies. One case at Johns Hopkins showed a 78-year-old patient with nortriptyline levels at 185 ng/mL-above the 150 ng/mL ceiling. Without TDM, the dose might have been increased. Instead, it was cut in half. No arrhythmia. No ICU stay.
When TDM Saves Lives
TDM doesn’t just prevent overdose. It helps doctors fine-tune treatment when standard dosing fails.Take a patient with chronic pain who’s been on amitriptyline for months but still feels no relief. Their level is 60 ng/mL-below the therapeutic range. The doctor knows it’s not about adherence. It’s about metabolism. Maybe they’re an ultrarapid metabolizer, clearing the drug too fast. Or maybe they’re taking an antibiotic that blocks the enzyme (CYP2D6) that breaks down TCAs. TDM gives the answer. The dose can be adjusted. Or a different drug can be chosen.
Conversely, a patient might feel fine but have levels at 220 ng/mL. No symptoms yet. But their ECG shows a borderline QRS widening. That’s a red flag. TDM catches it before they have a seizure or cardiac arrest. In one study, patients whose TCA levels were kept in range had a 35% lower risk of hospitalization compared to those adjusted only by symptoms.
Psychiatrists report real-world wins. One practitioner in a Reddit thread said they’d prevented three ICU admissions this year alone using TDM in elderly patients. Another nurse practitioner noted the biggest hurdle isn’t the test-it’s getting patients to come back for blood draws when they feel better. But skipping those draws is how people end up in emergency rooms.

The Hidden Problems with TDM
TDM sounds simple. But in practice, it’s messy.First, not all labs use the same reference ranges. One might say 200 ng/mL is the max. Another says 220. That’s a 15-20% difference. If your doctor doesn’t know which range their lab uses, they could misinterpret your results.
Second, 32% of TDM requests lack basic info-like what dose you’re on, when you last took the pill, or what other drugs you’re taking. That’s a huge problem. Medications like fluoxetine, bupropion, or even some heart drugs can block the enzymes that break down TCAs. Without knowing what you’re on, the lab result is useless.
Third, TDM doesn’t replace clinical judgment. One case in Clinical Toxicology described a woman with amitriptyline at 190 ng/mL-technically in range-but her QRS was widened to 140 ms. She needed immediate treatment. Her level wasn’t toxic. But her body was. That’s why doctors are taught: never rely on the number alone. Always look at the ECG. Always check symptoms. Always ask: Is this person acting like they’re overdosing?
Who Needs TDM Most
Not everyone on TCAs needs regular blood tests. But some groups absolutely do.- Elderly patients (over 65): Slower liver function means drugs build up. They’re also more sensitive to anticholinergic effects like confusion and urinary retention.
- Patients with liver disease: Even mild cirrhosis can cut TCA clearance by half.
- Those on multiple medications: Especially antidepressants, antifungals, or heart drugs that interact with CYP enzymes.
- People who haven’t responded to standard doses: TDM tells you if it’s a dose issue or a metabolism issue.
- Anyone with a history of cardiac issues: TCAs can worsen arrhythmias. Monitoring is non-negotiable.
For young, healthy adults with no other meds and no heart problems? TDM may be less critical-especially in the first few weeks. But if symptoms appear or treatment stalls, get the test.
The Future of TDM
New tools are making TDM faster and smarter.Siemens Healthineers just rolled out a handheld TCA monitor in Europe that gives results in 20 minutes-not two days. The FDA approved an AI platform called PsychX Analytics that combines your blood level, ECG data, and symptoms to predict toxicity risk. It’s not perfect yet, but it’s a step toward real-time safety.
Even more promising? Pharmacogenetic testing. About 32% of U.S. academic hospitals now test for CYP2D6 and CYP2C19 gene variants before starting TCAs. If you’re a poor metabolizer, you might start on half the usual dose. If you’re ultrarapid, you might need more. One trial showed this cut the time to reach stable levels by 40%. Fewer blood draws. Fewer mistakes.
And while TCA prescriptions have dropped by 80% since 2000, they’re still the go-to for 68% of neuropathic pain specialists and 41% of geriatric psychiatrists. That means TDM isn’t going away. It’s evolving.
What You Should Do
If you’re prescribed a TCA:- Ask your doctor if TDM is recommended for you. Don’t assume it’s automatic.
- Make sure your blood draw is timed correctly-right before your next dose, after at least five days of consistent use.
- Bring a full list of every medication and supplement you take. Even OTC ones.
- Ask for your results. Know your numbers. Understand the range your lab uses.
- If you feel dizzy, confused, or your heart races, get an ECG. Don’t wait for your next appointment.
TCAs can be life-changing. But they’re not safe by default. Their power comes with responsibility. Therapeutic drug monitoring isn’t bureaucracy. It’s the difference between healing and disaster. For the right patients, it’s the only way to use these drugs without risking their lives.
Is therapeutic drug monitoring required for all tricyclic antidepressants?
No, it’s not mandatory for everyone. But it’s strongly recommended for elderly patients, those on multiple medications, people with liver issues, and anyone with a history of heart problems. For healthy young adults with no risk factors, it may be optional during initial treatment-but still advisable if treatment isn’t working or side effects appear.
How often should TCA blood levels be checked?
The first test should be done after 5-7 days of steady dosing to confirm steady-state levels. After that, check every 3-6 months if you’re stable. More frequent testing is needed after dose changes, if you start or stop other medications, or if you develop new symptoms like dizziness, confusion, or irregular heartbeat.
Can I skip TDM if I feel fine?
Feeling fine doesn’t mean your levels are safe. Many people with toxic TCA levels report no symptoms until they suddenly collapse. Blood levels can creep up slowly due to aging, drug interactions, or changes in liver function. Skipping monitoring is like driving without a speedometer-you might be fine today, but you won’t know when you’re speeding toward danger.
What if my TCA level is in range but I still have side effects?
Side effects don’t always match blood levels. Some people are more sensitive to anticholinergic effects, even at normal concentrations. Others may have a metabolite that’s more active or toxic than the parent drug. Your doctor should consider your symptoms, ECG results, and possibly testing for metabolites like nortriptyline if you’re on amitriptyline. Don’t assume the number is the whole story.
Are there alternatives to blood tests for monitoring TCA levels?
Currently, blood tests are the only reliable method. New technologies like handheld monitors and continuous interstitial fluid sensors are in development, but they’re not yet standard. Some clinics combine TDM with pharmacogenetic testing to predict how you’ll metabolize the drug, which reduces the need for frequent blood draws. But you still need a baseline blood test to confirm predictions.

Written by Felix Greendale
View all posts by: Felix Greendale