If you're on warfarin, you know how frustrating it can be to get your INR numbers all over the place. One week you're perfectly in range, the next you're hovering at 4.5 or dipping below 2.0. It’s not just numbers on a screen-it’s anxiety, extra clinic visits, and the constant fear of a clot or a bleed. For many people, the answer isn’t changing their warfarin dose again. It’s something simpler, quieter, and surprisingly overlooked: vitamin K.
Why Your INR Keeps Fluctuating
Warfarin works by blocking vitamin K’s role in making clotting factors. But vitamin K doesn’t just come from your pill-it’s in your food. Spinach, kale, broccoli, Brussels sprouts, even some oils contain it. If you eat a big salad one day and then skip greens the next, your vitamin K intake swings wildly. That swings your INR. It’s not your fault. It’s how the drug works. Studies show that about 30 to 50% of people on warfarin have unstable INRs. That means they’re spending too much time outside the safe range-too high (risk of bleeding), too low (risk of stroke or clot). And for some, no matter how carefully they take their warfarin, their INR just won’t settle.How Low-Dose Vitamin K Fixes This
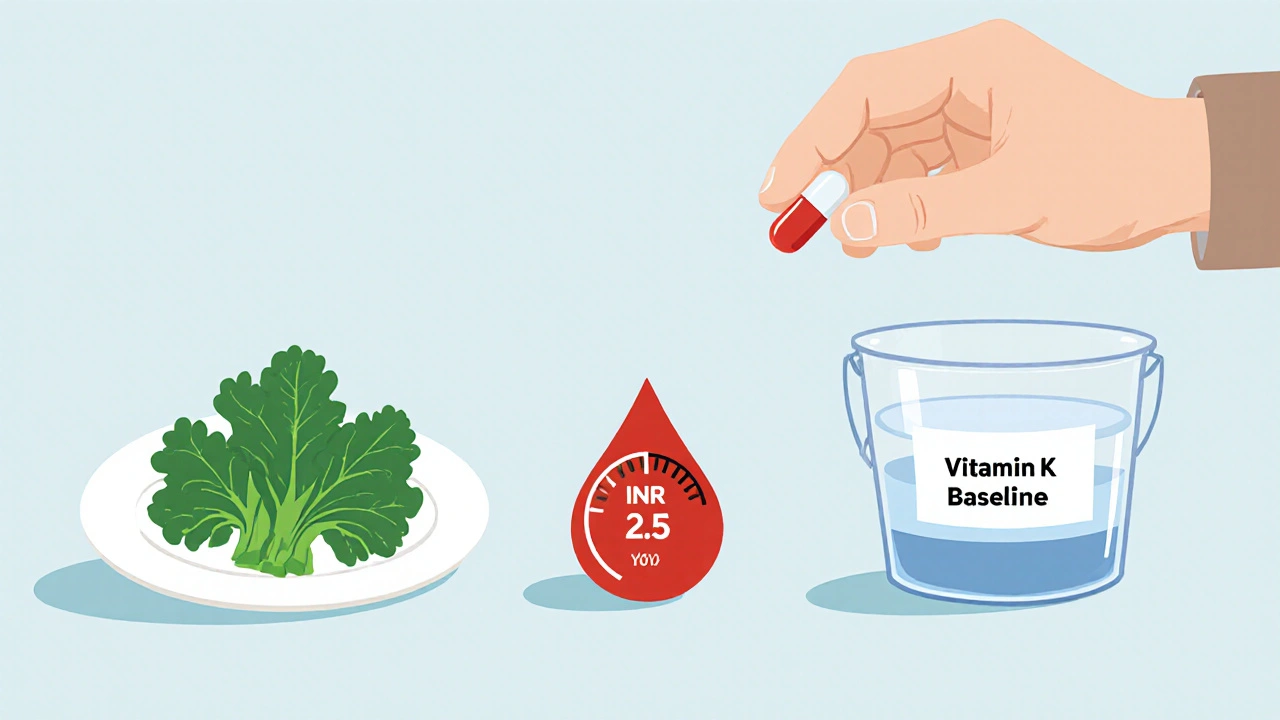
Here’s the counterintuitive part: taking a small, daily dose of vitamin K can actually make your INR more stable. Not because it cancels out warfarin. But because it removes the noise. Think of your body like a bucket. Warfarin is a slow leak. Vitamin K from food is a random hose turning on and off. Some days the hose is wide open (spinach smoothie), other days it’s off (fast food). The water level (your INR) goes up and down. Now imagine you turn the hose on just a little bit, every single day-150 micrograms. That’s about the amount in a small serving of kale. Suddenly, the baseline is steady. The big swings from food matter less. Research from 2007 and again in 2016 showed that patients taking 150 mcg of vitamin K1 daily had fewer extreme INR spikes and drops. One study found a 4% drop in dangerous INR excursions-meaning fewer times your INR went above 4.5 or below 1.5. That’s not just a number. That’s fewer hospital visits, fewer emergency doses, fewer scary moments.Who Should Consider This
This isn’t for everyone. If your INR is steady, you don’t need it. But if you’ve been on warfarin for a while and:- Your Time in Therapeutic Range (TTR) is below 65%
- You’ve had three or more INRs above 4.0 or below 1.5 in the last six months
- Your diet is inconsistent, even after trying to eat the same amount of greens
- Your doctor has ruled out other causes like medication interactions or alcohol use
What Dose to Take and How
The only dose proven in multiple clinical trials is 150 micrograms (mcg) of phylloquinone (vitamin K1) per day. That’s it. No more, no less. You can get this in a simple, inexpensive supplement. A 5 mg bottle of vitamin K1 (generic) costs about $8 at most pharmacies. One tablet divided into 33 pieces gives you 150 mcg. Or you can buy 150 mcg capsules online or at health stores. Take it at the same time every day-morning or night, doesn’t matter. But be consistent. Skip a day? Your INR might wobble again. Important: Don’t start this on your own. You need your doctor’s approval and regular INR checks. The first month is critical. Your warfarin dose might need to go up slightly-on average, by 0.5 to 1.5 mg daily-as your body adjusts to the steady vitamin K. That’s normal. It doesn’t mean the supplement isn’t working. It means it’s working.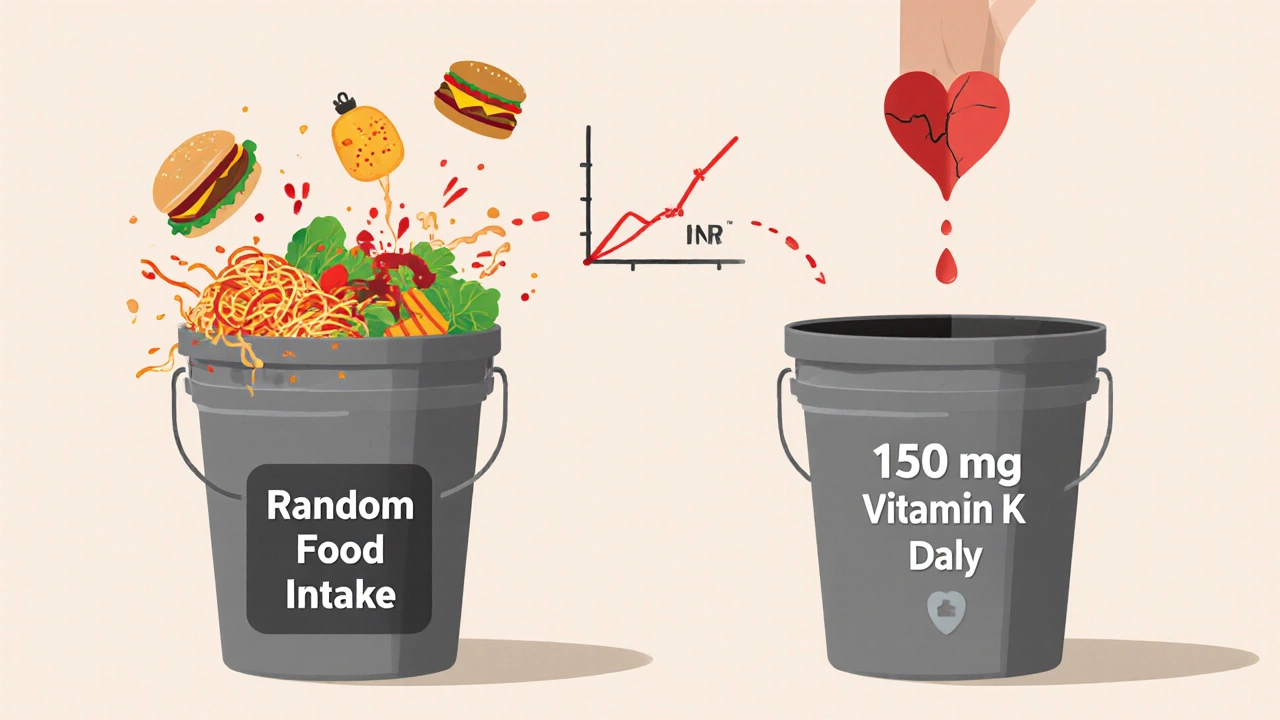
What to Expect
You won’t see results overnight. It takes 4 to 8 weeks for your INR to stabilize. In the first two weeks, your INR might dip lower than usual. That’s the lag effect. Your liver is adjusting. Your doctor will watch this closely and may reduce your warfarin dose temporarily. After that, most people report:- Fewer INR spikes and crashes
- Less need for emergency warfarin dose changes
- More confidence in daily life
What Doesn’t Work
Vitamin K supplementation won’t help if:- You’re already eating a ton of vitamin K-more than 500 mcg a day (think daily kale smoothies and big servings of broccoli)
- You miss warfarin doses regularly
- You have a mechanical mitral valve (requires higher INR targets, and vitamin K hasn’t been studied enough here)
- You’ve recently had a clot or major bleeding
How It Compares to Other Options
Many people ask: Why not just switch to a DOAC like Eliquis or Xarelto? Those drugs don’t need INR checks. And they’re great-for most people. But about 20% of patients on anticoagulants still need warfarin. That’s over 2 million people in the U.S. alone. DOACs aren’t safe for mechanical valves. They’re expensive. And they can’t be reversed easily in emergencies. Vitamin K is cheap, safe, and works with your existing treatment. Compared to home INR monitors (which cost $500-$1,000 and require training), vitamin K is passive. No device. No calibration. Just a daily pill.
What Doctors Say
Guidelines are cautious. The American College of Chest Physicians doesn’t formally recommend it yet. But they don’t say no either. The European Heart Rhythm Association calls it “promising but not yet definitive.” Still, more clinics are offering it. In 2019, only 15% of U.S. anticoagulation clinics provided vitamin K supplementation. By 2023, that number jumped to 28%. And with new trials expected to report results in 2024 and 2025, guidelines may change soon. One hematologist in Boston put it this way: “It’s not magic. But for patients who’ve tried everything else, it’s the most reliable tool we’ve got to bring stability back.”Real Stories
On Reddit’s r/Warfarin, users share their experiences: > “After 8 years of rollercoaster INRs, I started 150 mcg vitamin K daily. My TTR went from 55% to 78%. Only two INRs above 4.0 in six months. I finally feel in control.” > “My doctor tried it, but my warfarin dose went up from 3mg to 4.5mg. I’m not sure it was worth it.” The second case isn’t a failure-it’s a sign the vitamin K worked. The dose had to be adjusted. That’s normal. The Anticoagulation Forum tracked over 400 patients who tried it. Two-thirds saw improvement. One in ten got worse. But most of those cases involved poor adherence or too much dietary vitamin K.Bottom Line
If your INR is unpredictable, and you’re tired of the seesaw, ask your doctor about low-dose vitamin K. It’s not a cure. But for the right person, it’s a quiet, powerful way to take back control. You don’t need to eat less kale. You don’t need to buy expensive monitors. You just need a consistent, tiny dose of vitamin K every day-and a doctor who’s willing to adjust your warfarin with you. It’s not in every guideline. But it’s in the data. And for thousands of people, it’s the difference between living in fear and living normally.Can I take vitamin K supplements while on warfarin?
Yes-but only under medical supervision. Taking 150 mcg of vitamin K1 daily has been shown to stabilize INR in people with unexplained fluctuations. Never start or stop without talking to your anticoagulation clinic or doctor. Your warfarin dose will likely need adjustment.
Does vitamin K cancel out warfarin?
No. Vitamin K doesn’t cancel warfarin. It makes your body’s response to warfarin more predictable. Warfarin still blocks vitamin K’s clotting effects. But when you get a steady, small amount every day, your INR doesn’t swing wildly based on what you ate last night.
What’s the right dose of vitamin K for INR stability?
The only dose proven in clinical trials is 150 micrograms (mcg) of vitamin K1 (phylloquinone) per day. Higher doses can interfere with warfarin too much and cause dangerous INR drops. Lower doses don’t seem to help. Stick to 150 mcg.
How long does it take for vitamin K to work?
It takes 4 to 8 weeks to see stabilization. In the first 2-4 weeks, your INR may drop unexpectedly. This is normal. Your doctor will adjust your warfarin dose during this time. Don’t panic. Don’t skip doses. Just keep taking the vitamin K and get your INR checked as scheduled.
Can I get enough vitamin K from food instead of supplements?
You can-but only if you eat the same amount every single day. One day with a big salad and the next with pizza will still cause INR swings. Most people can’t maintain that consistency. Supplements give you control. You know exactly how much you’re getting.
Is vitamin K safe long-term?
Yes. At 150 mcg daily, vitamin K1 is extremely safe. The European Food Safety Authority says the safe upper limit is 10 mg per kg of body weight-meaning you’d need to take over 7,000 times this dose to risk toxicity. No major side effects have been reported in clinical trials.
Will vitamin K help if I have a mechanical heart valve?
It can. People with mechanical valves often have the hardest time stabilizing INR. While most trials excluded mitral valves, studies in aortic valve patients show clear benefit. If you’re stable on warfarin but your INR keeps drifting, vitamin K is worth discussing-even with a valve.
What if my INR gets worse after starting vitamin K?
That’s rare but possible. It usually happens if you’re eating too much vitamin K from food, missing warfarin doses, or have an underlying condition like liver disease or cancer. If your TTR drops after starting vitamin K, stop it and talk to your doctor. It’s not the supplement’s fault-it’s a sign something else is off.
Can I stop taking vitamin K if my INR gets stable?
Don’t stop without talking to your doctor. If you stop, your INR will likely swing again. Vitamin K isn’t a cure-it’s maintenance. Like wearing glasses, you need to keep taking it to stay stable. Some people stay on it for years.
Is vitamin K covered by insurance?
Usually not. Vitamin K1 supplements are sold as over-the-counter products, not prescription drugs. But they’re very cheap-often less than $0.01 per day. Most patients pay out of pocket. The cost is negligible compared to the cost of hospital visits from unstable INRs.

Written by Felix Greendale
View all posts by: Felix Greendale