Every year, tens of thousands of people end up in the hospital-not because their condition got worse, but because two medications they were taking clashed in ways no one warned them about. This isn’t rare. It’s common. And it’s preventable.
What Exactly Is a Drug Interaction?
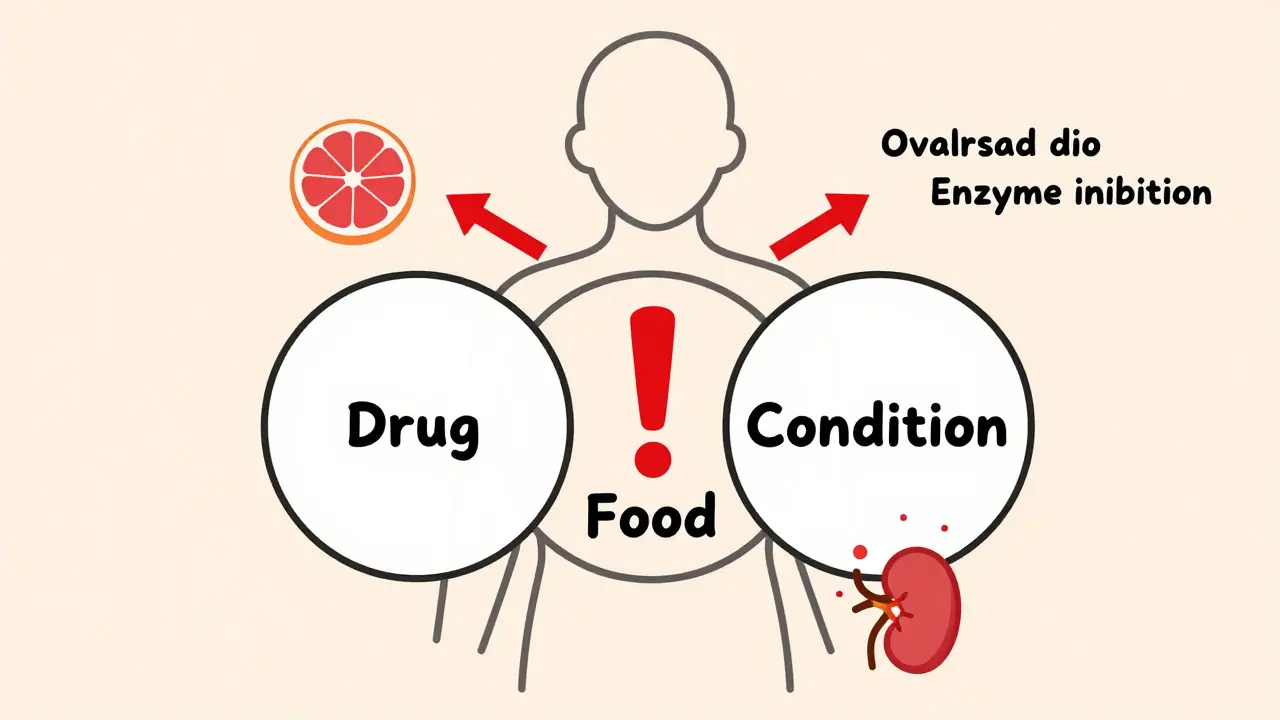
A drug interaction happens when something changes how a medication works in your body. It could be another pill, a food you eat, a supplement you take, or even a health condition you have. These changes can make a drug too strong, too weak, or cause unexpected side effects. It’s not just about mixing pills. Grapefruit juice can turn a safe dose of a cholesterol drug into a dangerous one. Calcium supplements can block your thyroid medicine from being absorbed. Even something as simple as drinking coffee at the wrong time can affect how your body handles certain medications.There are three main types of drug interactions:
- Drug-drug interactions: When one medication affects another. For example, taking the antibiotic clarithromycin with simvastatin (a statin) can cause muscle damage so severe it leads to kidney failure.
- Drug-food/drink interactions: When what you eat or drink changes how a drug is absorbed or broken down. Grapefruit juice is the most well-known offender-it interferes with an enzyme in your gut called CYP3A4, which breaks down about half of all prescription drugs. That means more of the drug enters your bloodstream than intended.
- Drug-condition interactions: When your existing health problem changes how a drug behaves. For instance, if you have kidney disease, your body can’t clear certain drugs like normal. That means even a standard dose might build up to toxic levels.
Why This Isn’t Just a Minor Risk
Drug interactions aren’t theoretical. They’re a leading cause of preventable harm. In the U.S., they contribute to 106,000 deaths every year-more than car accidents or diabetes complications. About 6.5% of all hospital admissions are linked to bad drug interactions, according to a 2022 study in JAMA Internal Medicine. That’s over 1.3 million emergency room visits and 350,000 hospital stays annually, costing the system more than $30 billion.Some medications are far riskier than others. Warfarin (Coumadin), a blood thinner, has more than 600 known interactions. Even something as harmless as cranberry juice or a common antibiotic like amoxicillin can throw off its effect. Too much warfarin? Risk of internal bleeding. Too little? Risk of stroke. Digoxin, used for heart rhythm problems, interacts dangerously with diuretics and certain antibiotics. Levothyroxine, the thyroid hormone replacement, won’t work properly if taken with calcium, iron, or even soy milk-unless you space them out by at least four hours.
And it’s not just older people. While those over 65 are at highest risk-taking an average of 4.7 prescriptions daily-young adults aren’t safe either. A 30-year-old taking birth control, an antibiotic, and a CBD oil supplement might not realize the combo could make their birth control fail. A teenager on ADHD meds and energy drinks might be pushing their heart rate into dangerous territory.
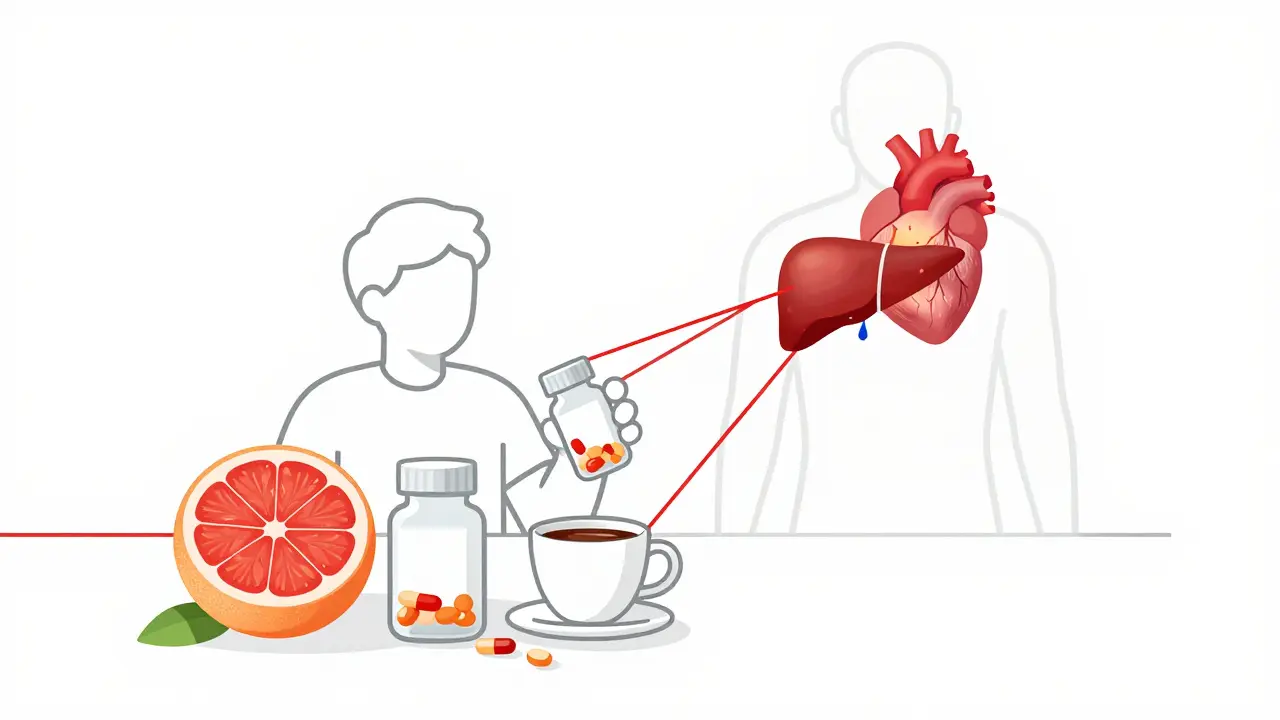
How Interactions Actually Happen in the Body
Most drug interactions happen in one of two ways: through how your body processes the drug (pharmacokinetic), or how the drug acts on your body (pharmacodynamic).Pharmacokinetic interactions deal with absorption, distribution, metabolism, and excretion. The liver enzyme CYP3A4 handles about 50% of all prescription drugs. If something blocks this enzyme-like fluconazole (an antifungal) or grapefruit juice-your body can’t break down the drug fast enough. Blood levels spike. That’s why taking simvastatin with fluconazole can raise its concentration by up to 2,000%. That’s not a typo. Two thousand percent. Result? Severe muscle breakdown, called rhabdomyolysis, which can destroy kidneys.
Pharmacodynamic interactions are about what the drug does to your body. Two sedatives taken together? You might fall asleep and not wake up. NSAIDs like ibuprofen can cancel out the blood pressure-lowering effect of diuretics by making your body hold onto salt and water. Beta-blockers can block asthma medications from working because they target the same receptors in your lungs.
Not all interactions are dangerous. Some are minor-like a mild stomach upset from taking a pill with food. But others are life-threatening. The key is knowing which is which.
Who’s Most at Risk-and Why
Elderly patients are the most vulnerable. They often take multiple medications for chronic conditions like high blood pressure, diabetes, arthritis, and heart disease. A 2022 AARP survey found that 42% of Medicare beneficiaries over 65 had at least one harmful drug interaction. The Beers Criteria, updated yearly by the American Geriatrics Society, lists 54 high-risk medications and combinations for older adults. Hospitals that follow these guidelines see a 27% drop in bad drug events.But it’s not just age. People with five or more chronic conditions are six times more likely to have a serious interaction. People taking drugs processed by CYP3A4, CYP2D6, or CYP2C9 enzymes-about 70% of all prescriptions-are at higher risk. That includes statins, antidepressants, blood thinners, painkillers, and many cancer drugs.
And here’s the hidden problem: fragmented care. One doctor prescribes a new medication. Another doesn’t know about it. Your pharmacist sees all your prescriptions-but only if you use the same pharmacy. A 2022 study in the New England Journal of Medicine found that 34% of patients leaving the hospital had at least one undocumented interaction risk because their doctors didn’t talk to each other.
How to Protect Yourself
You don’t need to be a doctor to avoid dangerous interactions. Here’s what actually works:- Keep a full list of everything you take. Not just prescriptions. Include over-the-counter meds (like ibuprofen or antacids), vitamins, herbal supplements (like St. John’s Wort or garlic pills), and even recreational substances like alcohol or cannabis. Write down the dose and how often you take it.
- Use one pharmacy. Chain pharmacies like CVS or Walgreens have systems that flag dangerous combinations. If you switch pharmacies, you lose that safety net.
- Ask your pharmacist. They’re the drug experts. Don’t wait for them to ask you. Bring your list every time you pick up a new prescription. Say: “Could this interact with anything else I’m taking?”
- Know your high-risk foods. Grapefruit juice is the big one. Avoid it if you’re on statins, certain blood pressure meds, or anti-anxiety drugs. Dairy and calcium supplements can block thyroid meds and antibiotics like ciprofloxacin. Take them at least 4 hours apart.
- Use a trusted interaction checker. The GoodRx Drug Interaction Checker is free and covers over 1,500 drugs. The NIH’s LiverTox database is great for liver-related risks. Medscape’s tool is used by 78% of U.S. doctors.
And if you’re on warfarin, digoxin, or levothyroxine-ask your doctor for a written interaction warning. Keep it in your wallet.
The Bigger Picture: Why the System Is Falling Short
Even with all the tech we have, the system is still broken. Only 25% of dangerous drug interactions are found during clinical trials-because those trials exclude older people, those with multiple conditions, and people taking other meds. That means drugs get approved based on ideal conditions, not real life.Pharmaceutical companies often downplay interaction risks in early studies. A 2022 study found that 73% of serious interactions are only discovered after the drug hits the market. That’s not negligence-it’s systemic. The FDA now requires interaction info on labels, but many patients never read them.
Electronic health records (EHRs) have drug interaction checkers built in, but only 42% of hospitals use systems that give real-time, severity-ranked alerts. The rest just pop up a generic warning. Doctors get so many alerts they start ignoring them. That’s called alert fatigue. And it’s deadly.
Meanwhile, the market for drug safety tech is exploding-projected to hit $7.8 billion by 2027. AI tools like IBM Watson are now scanning millions of clinical notes to find patterns no human could. In the future, your genetic profile might tell your doctor if you’re a slow metabolizer of certain drugs-before you even take them.
Final Thought: It’s Not About Fear. It’s About Awareness.
Drug interactions aren’t something to panic about. They’re something to manage. Most people take medications safely for years without issue. But one unnoticed interaction can change everything.Ask questions. Keep a list. Use one pharmacy. Talk to your pharmacist. Don’t assume your doctor knows everything you’re taking. Don’t assume a supplement is harmless. Don’t assume grapefruit juice is just a healthy breakfast.
Medication safety isn’t just about the pill in your hand. It’s about everything around it.
Can over-the-counter medicines cause drug interactions?
Yes. Common OTC meds like ibuprofen, naproxen, antacids, and even cold remedies can interact with prescription drugs. For example, ibuprofen can reduce the effect of blood pressure medications and increase the risk of stomach bleeding when taken with warfarin. Antacids with aluminum or magnesium can block absorption of antibiotics like ciprofloxacin and thyroid medications. Always check with your pharmacist before taking any OTC product with your regular meds.
Is it safe to take herbal supplements with prescription drugs?
Many herbal supplements are dangerous when mixed with medications. St. John’s Wort can reduce the effectiveness of birth control, antidepressants, and blood thinners. Garlic, ginkgo, and ginger can increase bleeding risk when taken with warfarin or aspirin. Ginseng can interfere with blood sugar control in diabetics. There’s no regulation for supplements, so their potency and ingredients vary. Always tell your doctor and pharmacist exactly what you’re taking-even if you think it’s "natural."
Why does grapefruit juice affect some drugs but not others?
Grapefruit contains compounds called furanocoumarins that block the CYP3A4 enzyme in your gut. This enzyme breaks down many drugs before they enter your bloodstream. If it’s blocked, too much of the drug gets absorbed. Not all drugs rely on CYP3A4, so grapefruit doesn’t affect them. Statins like simvastatin and atorvastatin are affected. Others like pravastatin are not. Always check your specific medication or ask your pharmacist.
Can alcohol interact with my medications?
Absolutely. Alcohol can increase drowsiness with sedatives, antidepressants, and painkillers. It can damage your liver when mixed with acetaminophen (Tylenol), raising the risk of liver failure. It can spike blood pressure when taken with some blood pressure meds, or cause dangerous drops in blood sugar with diabetes drugs. Even moderate drinking can be risky. If you’re on any regular medication, assume alcohol could interfere-unless your doctor says otherwise.
How often should I review my medications with a pharmacist?
At least once a year, or anytime you start, stop, or change a medication-even if it’s over-the-counter. If you see multiple doctors, schedule a medication review with your pharmacist every six months. Many pharmacies offer free consultations. Bring your complete list, including supplements and herbal products. This simple step can prevent a life-threatening interaction.
If you’re managing multiple medications, don’t wait for a crisis. Talk to your pharmacist today. Keep your list updated. Ask the hard questions. Your safety isn’t someone else’s job-it’s yours.

Written by Felix Greendale
View all posts by: Felix Greendale