Imagine your heart gets tired. Not the "end of a run and need a glass of water" tired, but really, bone-deep weary. That’s what left ventricular dysfunction (LVD) feels like—a sort of slow motion in the left ventricle, the heart’s main pumping chamber. For most people, finding out what's sapping their heart’s power doesn’t begin with guesswork or wild theories—it starts with a thin, flexible tube and a handful of surprising, life-changing facts about cardiac catheterization. Let's go deeper.
Unpacking Left Ventricular Dysfunction
Your left ventricle is supposed to take oxygen-rich blood in and push it out with a solid squeeze—supplying your organs, your head, your toes. But sometimes the squeeze is weak, for reasons ranging from high blood pressure to heart attacks or faulty valves. Millions of people in the UK and beyond live with LVD without knowing it at first. Doctors spot early symptoms like shortness of breath, leg swelling, and crushing fatigue, yet it’s easy to shrug them off as just "getting older." That’s where things get sneaky: LVD doesn’t yell; it just quietly steals your limits.
Current data from the British Heart Foundation estimate that nearly one million people in the UK alone show measurable signs of heart failure every year, many related to left ventricular dysfunction. The problem is, it’s not always clear what caused the dysfunction—was it a hidden blockage, a muscle that got damaged, or something else messing with the pumping force?
Doctors need to go beyond the stethoscope. Echocardiograms and blood tests get you partway, but to know exactly what’s happening, and to plan out treatment, the next step is invasive but super informative: cardiac catheterization. Why not just rely on scans? Because sometimes, the picture doesn’t show the full story—you need numbers, pressures, real-time responses, and, sometimes, a little detective work inside the heart arteries themselves.
What Happens During Cardiac Catheterization?
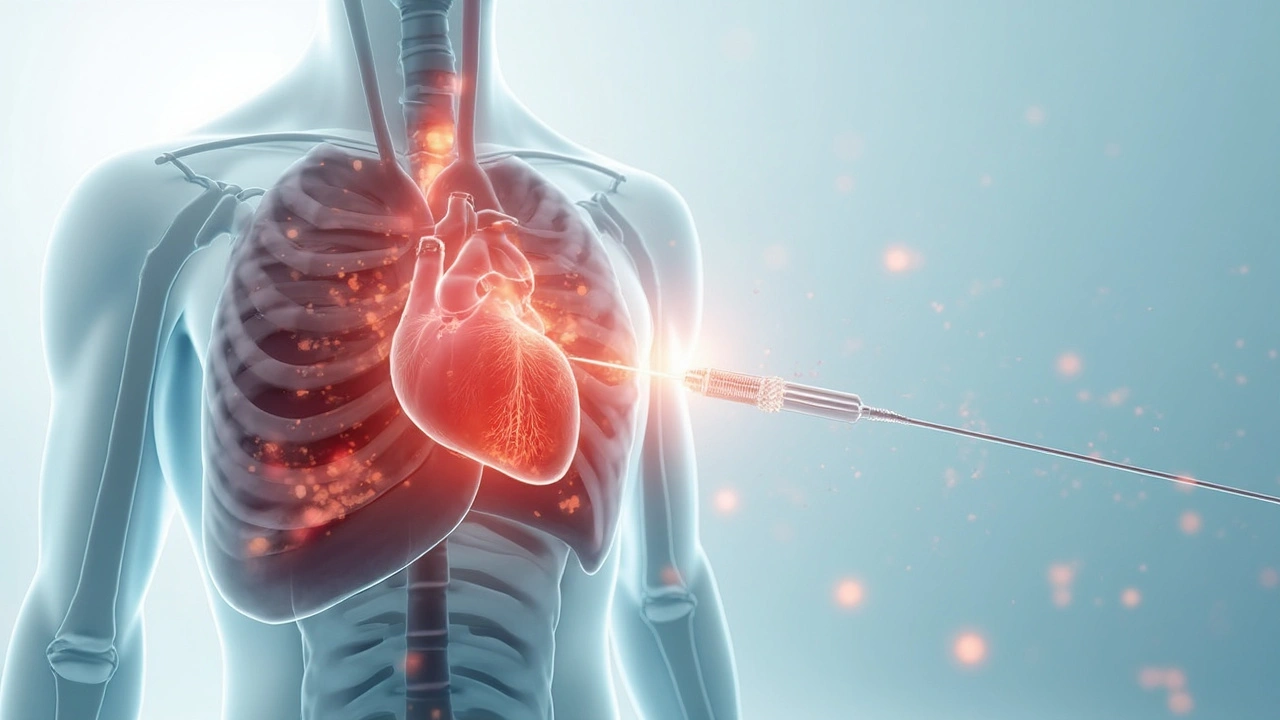
Picture this: you’re on a hospital bed under bright lights, a little nervous as a team in scrubs sets up machines. You’re awake, maybe a bit woozy, while a thin catheter (think a spaghetti strand, not a hosepipe) slides into your wrist or groin. Feels odd, but shouldn’t hurt thanks to the local anaesthetic. That’s the start of the magic.
Through that tube, doctors inject dye and capture live X-ray images—angiograms—watching blood flow and highlighting narrowings or clogs. They can also measure pressures directly in the left ventricle and other chambers. If they're trying to suss out if the ventricle is stiff, weak, or overloaded, they actually SEE it as it's happening. It's a level of detail that plain scans can’t match. One minute, you’ve got fuzzy symptoms and guesswork; the next, you have a map of your heart’s plumbing. That’s the power of cardiac catheterization.
While you're in the cath lab, a bunch of things are happening quietly in the background. The team watches for arrhythmias (weird rhythms), checks oxygen levels, and snaps dozens of pictures. Sometimes, cardiac output—the actual amount of blood the heart pumps each minute—gets measured using a special technique called thermodilution. Things can get high-tech fast: there's a whole world of pressure wires, fractional flow reserve (FFR) readings to test artery blockages, and even tests for how the heart muscle itself behaves under stress. This isn't just poking around. It's targeted, precise, and often over within an hour.
Why Cardiac Catheterization Makes the Difference in LVD
Let’s put numbers into focus. The left ventricular ejection fraction—the key metric for ‘how much blood gets pushed out with each beat’—sometimes hovers below 40% in people with heart failure. Doctors want to know: Is it low because the arteries upstream are clogged? Is there a muscle disease, or maybe hidden valve damage? Catheterization helps answer those questions, and sometimes solves them right then and there.
Here's a real edge: imagine a patient turns up with breathlessness and an echo shows a weak pump. The next steps shape the rest of their life. If the catheterization finds a treatable blockage, then a stent could fix the problem on the spot—preventing months or years of decline. Cardiac catheterization gives you a straight shot at finding out if blood isn’t reaching the heart muscle, which can sometimes be reversed if caught early. Sometimes, it's the difference between needing a lifetime of pills and facing a transplant down the line.
There's also a level of prediction here. By measuring the pressures inside the heart chambers and how they respond to tiny tweaks—like infusing special meds or fluids—doctors learn what kind of heart failure you have. Is it the kind that needs diuretics (fluid pills), or the kind that responds to increasing the squeeze? Is there a risk of sudden worsening? With catheterization, they're not guessing; they're targeting treatment.
Quick fact: In the UK, over 50,000 cardiac catheterizations are performed each year, and about a third are specifically focused on heart failure and LVD investigation, according to NHS stats from 2024. This isn’t a rare procedure—it’s the bread and butter of practical, life-saving cardiology.
The Treatment Side: Beyond Diagnosis
Think cardiac catheterization just tells doctors what’s wrong? That’s only half of it. The very same tube that’s diagnosing can often treat. The most dramatic example is opening a blocked artery, a procedure known as angioplasty. Imagine a balloon at the end of the catheter being inflated, smashing artery gunk away, and sometimes leaving behind a tiny wire cage—a stent—to keep things open. A brilliant fix for some cases of LVD where a blockage caused the heart muscle to weaken.
But it doesn't stop there. In certain patients, catheterization picks up dangerous valve leaks or pressure problems, and in the same sitting, interventional cardiologists can repair valves using special clips or replace them completely without open-heart surgery. The recovery time is way shorter, and the risks—especially for older or sicker patients—drop dramatically compared to traditional surgery.
Sometimes, catheterization helps doctors decide who really needs a pacemaker or even an implantable defibrillator. During the procedure, nerve conduction and heart rhythm are mapped, spotting those who might be one faint away from disaster. The information from a cath study shapes the whole downstream treatment plan: what drugs to use, whether beta-blockers make sense, when to add advanced heart failure medications, or who should see a heart transplant team.
To give you an idea of how quickly things can move, NHS audits show that patients diagnosed and treated with catheter-based interventions recover functional capacity up to 20% faster, and fewer end up re-hospitalized within one year compared to those managed with medications alone. There’s no substitute for a real-time, eyes-inside-the-heart approach.

Practical Tips, Patient Stories, and Looking Ahead
If you’re facing a cardiac catheterization, prepping makes a big difference. Don’t stop blood thinners or regular meds unless told by your doctor. Arrive with someone you trust for support (leaving solo, post-procedure, isn’t allowed). Expect to be awake but comfortable—none of those Hollywood moments where you’re out cold. Tell your care team if you’re allergic to shellfish or iodine, because contrast dyes matter.
Afterwards? You’ll likely need to rest for a few hours, especially if the groin route was used. Keep an eye out for swelling or pain at the entry site; rare, but something to tell a nurse. Drink extra water for the next day to flush out the dye. You might have a bruised area that looks worse than it feels—that’s normal. Complications—bleeding, infection, or rare reactions—are possible but less than 1% end up serious in the UK, according to 2024 Registry of Interventional Cardiology data.
Let’s look at real experience. Alan, a 62-year-old builder from Sussex, put off shortness of breath until one bad day at the pier. He landed in the hospital, and within hours, a catheterization found a tight narrowing in his main artery. One stent later, Alan was walking three miles a day again. Lisa, a 39-year-old artist from Hove, found her fatigue wasn’t "just stress." A catheter study spotted a rare valve flapping the wrong way. A simple, low-risk catheter valve fix and she’s back to painting.
So, what’s next for catheterization? The future is all about smaller, smarter, and safer. We’re seeing the first whispers of robotic-assisted caths for higher precision, new sensors that map electrical flow in 3D, and biodegradable stents that disappear after their job is done. Researchers are even exploring using catheters to deliver stem cells or gene therapy, aiming to actually repair weak hearts—science fiction that might be real by the next Brighton Marathon.
Here’s a quick comparison for the numbers people:
| Aspect | Cardiac Catheterization | Non-Invasive Imaging |
|---|---|---|
| Diagnostic Accuracy for LVD | 95%+ | 75-85% |
| Treatment Capability During Procedure | Yes | No |
| Risk of Major Complications | Less than 1% | Negligible |
| Recovery Time | 3-6 hours | None |
| Availability in UK NHS Centers | All major hospitals | All |
So, when you hear about cardiac catheterization for left ventricular dysfunction, you’re not just hearing about a test—you’re hearing about the difference between guessing and knowing, between watching and doing. It’s the tool that lets doctors not just see your problem, but fix it before your heart gives up. That’s medicine, but it’s also hope—and every ounce of hope counts when your heart needs a break.


Written by Felix Greendale
View all posts by: Felix Greendale