Heartburn during pregnancy isn’t just annoying-it can feel unbearable. If you’re pregnant and lying awake at night with a burning sensation in your chest, you’re not alone. Up to 80% of pregnant people experience heartburn, especially in the second and third trimesters. Hormones relax the valve between your stomach and esophagus, and as your baby grows, they push up on your stomach, forcing acid back up. It’s a physical reality of pregnancy, not a sign something’s wrong. But when lifestyle changes aren’t enough, many turn to medications. The big question: Which ones are actually safe?
First-Line Defense: Antacids Like Tums
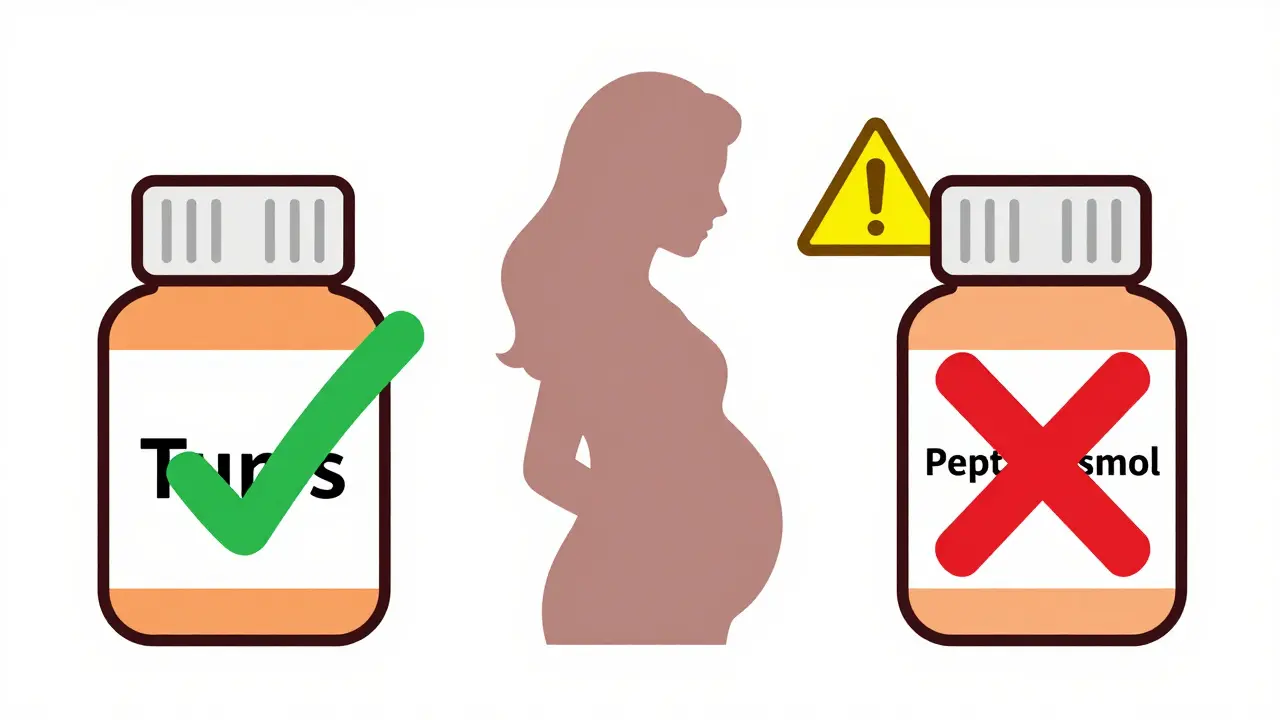
When it comes to heartburn relief in pregnancy, antacids are where most doctors start. And for good reason. Calcium carbonate-based antacids-like Tums, Rolaids, and some generic brands-work fast. They neutralize stomach acid right where it’s causing trouble, giving you relief in minutes. The best part? Calcium is something your body needs during pregnancy anyway. Your baby’s bones and teeth are forming, and your own calcium stores are being drawn on. Tums don’t just soothe your heartburn-they help replenish what your body’s using up.Not all antacids are created equal. Avoid products with aluminum hydroxide or magnesium trisilicate. Aluminum can build up in your system and isn’t recommended during pregnancy. Magnesium trisilicate has been linked to possible complications in animal studies, and while human data is limited, it’s not worth the risk. Mylanta is okay if it’s the version without trisilicate, but always check the label. And never, ever use Pepto-Bismol. It contains bismuth subsalicylate, which is related to aspirin-and aspirin is a hard no during pregnancy because of bleeding risks and potential effects on the baby’s heart and lungs.
How much is too much? Stick to the recommended dose: 500-1500 mg of calcium carbonate every 4 to 6 hours as needed. Don’t go over 7,500 mg total per day. Long-term, high-dose use can lead to kidney stones or electrolyte imbalances. If you’re taking Tums daily for weeks, talk to your provider. They might suggest switching to something else or checking your calcium levels.
Second-Line: H2 Blockers Like Pepcid
If antacids aren’t cutting it-maybe you’re getting heartburn multiple times a day, or it wakes you up at night-your provider might suggest an H2 blocker. These drugs don’t neutralize acid. Instead, they tell your stomach to make less of it. Famotidine (Pepcid) is the go-to here. It’s been studied more than any other H2 blocker in pregnancy, and the data is reassuring. Studies show no increased risk of birth defects, preterm birth, or low birth weight. It starts working in about an hour and lasts up to 12 hours, which makes it great for nighttime relief.Ranitidine (Zantac) used to be a popular choice-but it was pulled from the U.S. market in April 2020 because it was found to contain NDMA, a probable carcinogen. Even if you still have some lying around, don’t use it. It’s no longer considered safe, even outside of pregnancy.
H2 blockers are generally well-tolerated. Some people report mild side effects like headaches or dizziness, but that happens in only 3-5% of users. They’re considered safe for short-term use during pregnancy. If you’re taking Pepcid for more than a couple of weeks without improvement, it’s time to reassess. Maybe you need a stronger option-or maybe your symptoms aren’t just heartburn.
Third-Line: Proton Pump Inhibitors (PPIs) Like Prilosec
PPIs are the strongest acid reducers available over the counter. Omeprazole (Prilosec), lansoprazole (Prevacid), and pantoprazole (Protonix) block the final step of acid production in your stomach. They’re powerful. They last longer than H2 blockers-up to 24 hours or more. But they’re not your first pick.Why? Because while omeprazole is the most studied PPI in pregnancy and appears safe, there are still some unanswered questions. A 2019 study in JAMA Pediatrics found a small, possible link between PPI use in the first trimester and childhood asthma. That doesn’t mean PPIs cause asthma. It just means the association needs more study. For that reason, most providers hold off on PPIs until after the first 12-14 weeks, when the baby’s major organs are done forming. If you’re still struggling with heartburn after trying antacids and H2 blockers, your doctor might say it’s okay to try omeprazole. But only if the benefits clearly outweigh the unknowns.
Long-term use of PPIs-even outside of pregnancy-can affect how your body absorbs calcium, magnesium, and vitamin B12. That’s why they’re not meant to be taken daily for months or years without monitoring. In pregnancy, the goal is always the shortest possible duration at the lowest effective dose.
When to Avoid Medications Altogether
The first trimester is the most sensitive time. That’s when your baby’s organs are forming. Even if a medication is considered low-risk, the safest choice is often no medication at all. The American College of Obstetricians and Gynecologists (ACOG) and multiple OB/GYN groups recommend trying non-drug approaches first during the first 14 weeks of pregnancy.Here’s what works:
- Eat smaller meals-five or six a day instead of three big ones.
- Avoid trigger foods: spicy, fried, fatty, chocolate, citrus, coffee, and carbonated drinks.
- Don’t lie down for at least three hours after eating.
- Wear loose clothing-tight waistbands make pressure worse.
- Sleep with your head elevated. Use a wedge pillow or stack a couple of regular pillows under your mattress.
- Chew gum after meals. It increases saliva, which helps neutralize acid.
If you’re still having trouble after trying all of this, then it’s time to talk to your provider about medication. Don’t wait until it’s unbearable. But don’t reach for the medicine cabinet without checking first.
What Doesn’t Work-and What Could Harm
Some common remedies are dangerous during pregnancy. Pepto-Bismol is the biggest red flag. It’s not just “not recommended”-it’s actively discouraged because of its aspirin-like component. The same goes for any product with salicylates.Also avoid herbal remedies unless your provider approves them. Ginger tea is generally safe and can help with nausea, but some herbal teas (like chamomile, peppermint, or licorice root) may affect hormones or uterine contractions. Don’t assume “natural” means safe.
And while antacids are usually fine, don’t combine them with iron supplements unless your provider tells you to. Calcium can interfere with iron absorption. If you’re taking prenatal vitamins with iron, take them at least two hours apart from your antacid.
What to Do If Symptoms Don’t Improve
Heartburn is common. But if you’re having trouble swallowing, vomiting blood, losing weight, or having chest pain that radiates to your arm or jaw, that’s not just heartburn. It could be something more serious-like a hiatal hernia, gastritis, or even a heart issue. Don’t brush it off.Also, if you’ve tried antacids, H2 blockers, and lifestyle changes for two weeks and nothing helps, talk to your OB/GYN or ask for a referral to a gastroenterologist. Sometimes, what feels like heartburn is actually bile reflux or another condition that needs different treatment.
And remember: just because a medication is sold over the counter doesn’t mean it’s risk-free in pregnancy. Always check with your provider before starting anything new-even if it’s been safe for your friend or your sister-in-law. Every pregnancy is different. Your body, your baby, your needs-they’re unique.
Bottom Line: Safety First, Relief Second
The safest approach to heartburn in pregnancy is simple: start with lifestyle changes. If that’s not enough, reach for calcium carbonate antacids like Tums. If you still need more, famotidine (Pepcid) is your next best option. Save PPIs like omeprazole for when nothing else works-and only after your first trimester. Avoid anything with aspirin, aluminum, or trisilicate. And never take anything without talking to your provider first.Heartburn doesn’t mean you’re doing something wrong. It’s just part of the journey. But how you manage it matters-for your comfort, your health, and your baby’s development. You don’t have to suffer. But you do need to choose wisely.


Written by Felix Greendale
View all posts by: Felix Greendale